
- Home
- India
- World
- Premium
- THE FEDERAL SPECIAL
- Analysis
- States
- Perspective
- Videos
- Sports
- Education
- Entertainment
- Elections
- Features
- Health
- Business
- Series
- In memoriam: Sheikh Mujibur Rahman
- Bishnoi's Men
- NEET TANGLE
- Economy Series
- Earth Day
- Kashmir’s Frozen Turbulence
- India@75
- The legend of Ramjanmabhoomi
- Liberalisation@30
- How to tame a dragon
- Celebrating biodiversity
- Farm Matters
- 50 days of solitude
- Bringing Migrants Home
- Budget 2020
- Jharkhand Votes
- The Federal Investigates
- The Federal Impact
- Vanishing Sand
- Gandhi @ 150
- Andhra Today
- Field report
- Operation Gulmarg
- Pandemic @1 Mn in India
- The Federal Year-End
- The Zero Year
- Science
- Brand studio
- Newsletter
- Elections 2024
- Events
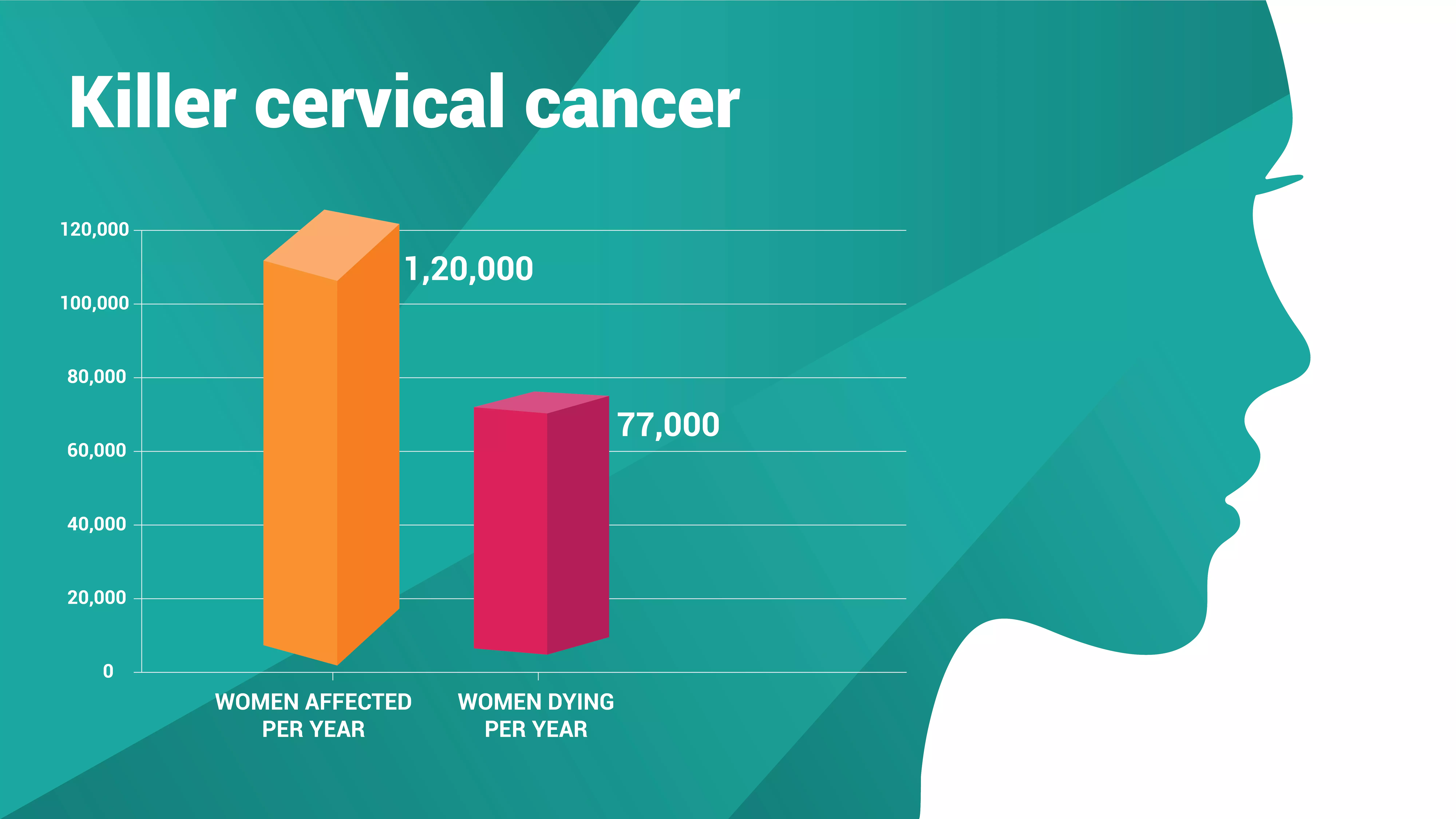
How vaccine rollout can save lives of 77,000 women dying of cervical cancer every year in India

A few days ago, news media went abuzz that the central government is set to roll out a human papillomavirus (HPV) vaccination campaign for girls in the 9-14-year age group by April 2024 in a bid to prevent the incidence of cervical cancer, which is the second-most-common cancer among women in India.Alas, within days of the news coming out, dismissing the reports, the Union Ministry of...
A few days ago, news media went abuzz that the central government is set to roll out a human papillomavirus (HPV) vaccination campaign for girls in the 9-14-year age group by April 2024 in a bid to prevent the incidence of cervical cancer, which is the second-most-common cancer among women in India.
Alas, within days of the news coming out, dismissing the reports, the Union Ministry of Health clarified that the government has not yet taken any decision regarding the vaccine rollout, making India miss the target of eliminating cervical cancer by 2030.
The Director-General of the World Health Organisation, Tedros Adhanom Ghebreyesus, made a global call to eliminate cervical cancer, and the World Health Assembly adopted the Global Strategy for cervical cancer elimination in August 2020. The fundamental strategy is called 90-70-90, which means 90% of girls are fully vaccinated with the HPV vaccine by the age of 15, 70% of women screened using a high-performance test by the age of 35, and again by the age of 45 and 90% of women with pre-cancer treated and 90% of women with invasive cancer managed. With this, an incidence rate of less than 4 per 1,00,000 women is expected to be achieved by 2030. In this global strategy, screening and treatment are like mopping a wet floor; vaccination is akin to closing the leaking tap.
Cervical cancer is the second-most prevalent cancer among women in India, and every year around 1,20,000 women are affected. Nearly 77,000 women die yearly due to cervical cancer.
“Internationally, mass vaccination drives have shown to be reasonably effective in increasing the coverage of HPV vaccination, which is crucial in preventing cervical cancer. Developed countries like Australia and the Scandinavian countries have a very high level of success, not only in girls but boys as well,” says Ravi Mehrotra, Rollins School of Public Health, Emory University, Atlanta, GA USA.
What is cervical cancer?
Cancer, in simple words, is cells that grow out of control. Often, cancer is named after the body part where it germinates. As the name suggests, cervical cancer initiates when some cells in the cervix, the canal that connects the vagina to the upper part of the uterus, become cancerous. Hu-man papillomavirus (HPV) triggers the onset of cervical cancer. The infection per se does not re-sult in cancer, but if the virus persists for longer time, it results in development of cancer.
HPV is transmitted sexually from person to person. It is so common that nearly half of us will en-counter HPV at least once in our lifetime. Nevertheless, our immune system is adequate to ward off the virus and prevent infection. However, in a small number of women, less than one per cent, the virus lurks inside for many years and triggers cancer in a few cells in the cervix. As the trans-mission route of the HPV virus is sex, cancer develops only in women over the age of 30. Mostly, women are the victims; nevertheless, in rare cases, men, too, can be affected by HPV.
Risk factors for another type of cancer go up with age; thus, it is mainly the old who fall prey to other types of cancer. However, cervical cancer strikes early. The incidence rises in 30-34 years of age and peaks at 55-65 years, and the bulk of the cervical cancer patients are about 38 years of age.
Human papillomavirus
HPV is a member of the family Papillomaviridae. Scientists have discovered more than a hundred species, often called 'types', that infect mammals and some vertebrates, such as birds, snakes, tur-tles, and fish. Among the human papillomavirus, the emergence of more than 100 serotypes, dis-tinct variants within the species, has been discovered so far.
The good news is that only 10-20 variants can trigger cancer. The rest can, at worst, activate geni-tal warts. Among those variants that provoke cancer, nearly 80% of worldwide infections are by the HPV-16 and HPV-18 variants. The same is the case for cervical cancer in Indian women.
Although sexually transmitted, barrier methods such as condoms do not confer adequate protection from the HPV infection. Most of the infected do not show any symptoms. In rare cases, symptoms, such as warts on the genital area, are present. In some women, the virus lurks, sneering into the cells that sheath the surface of the cervix, called epithelial cells. They stay there for many years, slowly altering the cells and making them cancerous.
PAP test
A cervical PAP test, also called a Pap smear, would show the infection early on. With current treatment procedures, most women can be cured. It is important to remember, if one tests positive, it does not automatically mean cancer. The infection may have just occurred, and it gives a chance to prevent the onset of cancer.
During the pap smear test, named after Georgios Papanikolaou (a Greek physician who invented the test in the 1920s), a few sample cells are collected from the cervix using a soft brush and a flat scraping device. It does not cause any pain or cramping, but a few women may have minor bleed-ing. The sample cells are later examined under the microscope to see if any cells show typical can-cer symptoms. The test can also detect cell changes that suggest cancer may develop in the future.
Once the precancerous stage is detected, with the known medical intervention, we have a high chance to halt the progress of the onset of the cancer.
The vital part is to detect early. Regular periodic screening of all women in the age group is neces-sary to do so.
Screening
Only some individuals come forward for voluntary routine screening. It is only with large-scale routine screening that cervical cancer can be eliminated. Regular and periodic screening is arduous in countries like India, with large populations and most living in remote villages.
Screening and treatment are like mopping a wet floor. The root cause of the spillage is a broken tap. If the mopping and treatment of cervical cancer have to be fruitful, then one needs to fix the tap, that is, prevent the HPV infection.
Vaccine forestalls infection
Globally, there are two effective vaccines against HPV. Both use the same technology, Recombinant DNA technology, to develop the vaccine.
Like the aloo bonda, which has a cover made out of gram flour (besan) and filled with aloo masala, the HPV virus has a capsid covering its genetic materials. A capsid is nothing but a protein shell of a virus, enclosing its genetic material. The HPV capsid is made from a protein called L1.
The structure crumbles when we remove the shirt, but the helmet retains its shape. Likewise, the L1 protein can self-assemble into the size and shape of the virus, called virus-like particles (VLPs), even without the central genetic material inside.
How the vaccines work.
Just by smelling a piece of clothing with the criminal’s scent the police tracking dog can follow the odour and track the path taken by the fugitive. Likewise, our immune system requires only the scent of the virus, called antigen, to mount an attack and create the right sort of antibodies to fight the virus.
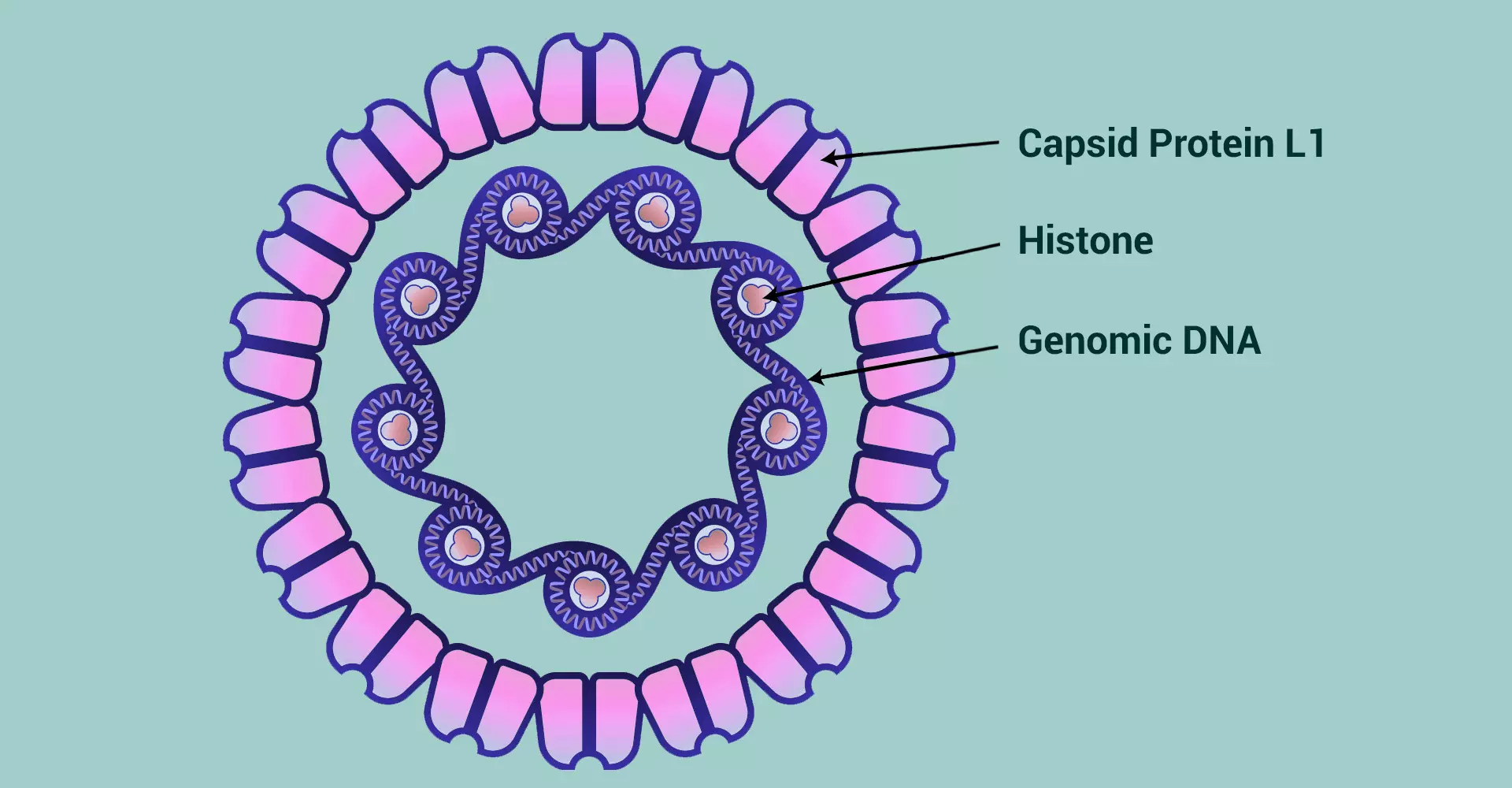
The vaccines approved in India use a dog-tracking strategy to identify the HPV virus in the human immune system. The genome of ordinary yeast that we use for cooking is modified. The gene for that code, the HPV capsid protein L1, is inserted into the yeast genome. The modified yeast pro-duces the HPV capsid protein L1. The capsid particles are sorted and purified. This particle is given an inoculation.
Once inside our body, the virus-like particles will trigger the immune system’s alarm bells. Alerted that foreign germs have gained entry, various arms of the human immune system, like B cells and T cells, are primed. They try to assess the identity of the intruder. The immune system responds by developing a neutralising antibody that detects, traces, and eliminates the germ. In the case of HPV, the immune system responds by a coating that inhibits the capsid protein L1 from peeling open. The viral genetic material cannot come out if the capsid cannot open. It is like castrating the virus.
Once we learn a new word, it usually becomes part of our vocabulary repository. Likewise, once the immune system develops neutralising antibodies, then the identity of the germ is always re-membered. Next time the same germ tries to take a foothold and infect, the reaction from the im-mune system is resolute, swift and robust. The germ is no longer able to play havoc.
Vaccines prevent the illness from becoming severe; it does not usually cure those already affected. Thus, vaccines are sweet to girls who are yet to attain puberty. However, vaccination is useless for those who have been infected.
A good vaccination programme must invariably accompany mass screening and treatment pro-grammes. That is why WHO's 90-70-90- the programme to eliminate cervical cancer by 2030.
Vaccines in India
After due process, the Gardasil-4 Quadrivalent vaccine was approved in India in 2008. This vac-cine targeted four variants of HPV viz HPV-6, HPV-11, HPV-16, and HPV-18. An improved ver-sion, Gardasil – 9 – Nonvalent vaccine, was permitted in 2018. This vaccine is effective against nine variants; HPV-6,HPV-11,HPV-16, HPV-18 HPV- 31, HPV-33, HPV-45, HPV-52, and HPV-58.
As these vaccines were imported, the cost was prohibitive for the mass immunisation programmes. Therefore, the Department of Biotechnology (DBT) encouraged the development of indigenous vaccines. With the support of the DBT, the Serum Institute of India introduced an indigenous HPV vaccine called CERVAVAC, a two-dose Quadrivalent vaccine. This vaccine, approved in 2023, offers protection against four high-risk variants: HPV-6, HPV-11, HPV-16, and HPV-18.
Cervarix, a bivalent vaccine targeting very high-risk variants HPV-16 and HPV-18, was initially marked in India and has been discontinued.
“Several vaccines are available in the Indian market. All these vaccines have shown a high effica-cy in preventing cervical cancers caused by the viruses they target,” says Ravi Mehrotra. “It is highly recommended for girls to get vaccinated against HPV. The vaccine is most effective when given before girls become sexually active, ideally between the ages of 9 and 14. The vaccine not only protects against cervical cancer but also against other cancers like anal, vulval, vaginal, oropharyngeal cancers as well as some cancers of the head and neck.” he added.
New variants
Viruses mutate, and new variants emerge. The vaccines may or may not offer the same level of protection against the new variant. “The current HPV vaccines are designed to protect against the most common high-risk HPV strains responsible for cervical cancer. If new strains of HPV emerge, the efficacy of the current vaccines would depend on the degree of cross-protection they offer against these new strains,” says Ravi Mehrotra.
Will we miss the date?
India aims to achieve 90-70-90 by 2030, just six years from now. There are several challenges be-fore India in achieving this goal. Massive screening is critical; most infected women are asymptomatic even after they develop precancerous cells. But where are we in terms of screening? According to the NFHS (National Family Health Survey) report, 2020, the percentage of women who have ever undergone cervical cancer screening in India is just 1.9% (2.2% urban and 1.7% rural). The women are unaware of the impending calamity as there are no symptoms. By the time the physicians identify, the game is over.
Lack of screening affects the survival rate. Adding to the woe, the early marriage of girls in India is adding an extra burden. About 23% of girls were married before the age of 18 and hence are at higher risk of cervical cancer in the absence of vaccination. The treatment of cervical cancer has miles to go. A recent study by Lancet, a reputed medical journal, shows that cervical cancer five-year survival was only 51.7% in India. The urban regions have higher survival rates compared to rural and northeast India.
The vaccination record is dismal. According to NFHS 2020, only 1% of girls aged between 9 years and 14 years have been inoculated for cervical cancer.
The press reports attributing the death of seven tribal girls to the HPV vaccine clinical trial in 2010 are still fresh in public memory. The Indian Parliament’s Standing Committee on Health conclud-ed that the “safety and rights of children were highly compromised and violated”. Following the uproar, Cervarix was discontinued in India. This blot is sure to evoke public sentiment and lead to vaccine hesitancy. Convincing the public and earning their trust will be another vital challenge for universal immunisation of girls for cervical cancer.
But if there is a will, there is a way. Sikkim did it. It showed that we can do it. The state govern-ment of Sikkim introduced the HPV vaccine for girls aged 9-13 in 2018-19. The two doses were provided complimentary. The state mobilised teachers, health staff, community health workers and public voices and organised a massive advocacy and awareness social mobilisation. It won the public trust, and 97% of the girls were administered both doses.
“Multi-level interventions beyond education alone can increase the uptake of the HPV vaccine,” says Ravi Mehrotra.
It is tragic that so many young women must die of what essentially is a curable disease; so many young girls should contract the infection in the first place, which is essentially preventable.
Will our governments wake up?
