- Home
- News
- Analysis
- States
- Perspective
- Videos
- Education
- Entertainment
- Elections
- World Cup 2023
- Features
- Health
- Business
- Series
- Economy Series
- Earth Day
- Kashmir’s Frozen Turbulence
- India@75
- The legend of Ramjanmabhoomi
- Liberalisation@30
- How to tame a dragon
- Celebrating biodiversity
- Farm Matters
- 50 days of solitude
- Bringing Migrants Home
- Budget 2020
- Jharkhand Votes
- The Federal Investigates
- The Federal Impact
- Vanishing Sand
- Gandhi @ 150
- Andhra Today
- Field report
- Operation Gulmarg
- Pandemic @1 Mn in India
- The Federal Year-End
- The Zero Year
- Premium
- Science
- Brand studio
- Home
- NewsNews
- Analysis
- StatesStates
- PerspectivePerspective
- VideosVideos
- Entertainment
- ElectionsElections
- Sports
- Loading...
Sports - Features
- BusinessBusiness
- Premium
- Loading...
Premium
Immunisation and efficacy: The saga of Covaxin
Covaxin is a class of time tested vaccines that has a good track record of generating long-lasting immunity for many different virus-caused diseases, such as flu, polio, and yellow fever.

Frightened by the heart-wrenching scenes of overwhelmed hospitals, medical oxygen scarcity and makeshift crematoriums resulting from the second wave’s uncontrolled rage, the day CoWIN portal was opened for 18-44 years age cohort to enrol for vaccination, 133 million citizens enthusiastically registered. Alas, the day the vaccination drive was to commence, stocks went empty at most...
Frightened by the heart-wrenching scenes of overwhelmed hospitals, medical oxygen scarcity and makeshift crematoriums resulting from the second wave’s uncontrolled rage, the day CoWIN portal was opened for 18-44 years age cohort to enrol for vaccination, 133 million citizens enthusiastically registered. Alas, the day the vaccination drive was to commence, stocks went empty at most vaccine centres.
Currently, the Serum Institute of India (SII) produces around 60 million doses a month, and is expected to raise capacity up to 100 million from July. Bharat Biotech is making 10 million doses a month which they hope will be ramped up to 100 million per month by September.
One lakh (0.1 million) doses of SputnikV, the vaccine from Russia, have arrived. India will become a production hub for SputnikV, and initially, about 50 million doses per month are expected to be produced.
Not all of these would be available for Indian use, as these firms have commitments abroad. Further, India cannot resist the export of vaccines as it needs vaccine ingredients from other countries. As the world’s largest vaccine manufacturer, India has a moral commitment to provide to the world.
Amid this, India has fallen in the rate of issuing vaccines. From the initial doses of 41 lakhs (4.1 million) from Feb 27 to Mar 5, the doses administered per week steadily went up to 247 lakhs (24.7 million) during the week of 3-9th April. However, since then, the trend has been downward, reaching 123 lakh (12.3 million) doses between 24-30th of April 2021.
The decrease is mainly due to non-availability of vaccine doses, although hesitancy also plays a part. With barely 2% of India’s 135 crores (1.35 billion) population vaccinated, and with an estimated 90 crore (0.9 billion) people above the age of 18 waiting for the jabs, at this rate, it would take years before the vaccine could be provided to all.
License to reproduce
Taking suo motu cognisance of the shortages, the Supreme Court, echoing the demand raised by the Left parties, remarked: “This is a public health emergency. Your affidavit says you have 10 PSUs who can manufacture. You can get licences through patent controller and get it manufactured…”
In the light of the SC’s remarks, the Indian patent acts and the intellectual property rights related to Covaxin developed with funding by the National Institute of Virology under the Indian Council of Medical Research (ICMR-NIV) have come into scrutiny.
Murali Neelakantan, a leading law expert, says as per rule 233 of General Financial Rules, 2017, all IPR resulting from government funding will rest with it.
The isolation, culture, and initial evaluation of the inactivated virus were fully funded by ICMR. Animal studies were conducted with joint funding from ICMR and Bharat Biotech International Limited (BBIL). The phase I, II and III clinical trials are wholly financed by BBIL.

Suppose the government of India is the rightful owner of the IPR, in that case, there is nothing to stop it from involving PSUs and other private manufacturing firms from producing Covaxin.
Even otherwise, the central government has powers to invoke Section 92 of the Patents Act, which permits the issue of compulsory licence, as the Left parties have pointed out, even without the patent holder’s consent, in the event of a national emergency.
In this case, the government can hustle all the capable PSUs and other willing private manufacturers to produce Covaxin and even Covishield for distribution to its citizens.
ICMR has come out with the statement that it has entered into a public-private partnership deal under which BBIL will have to pay a royalty for the production and sale of Covaxin. While the finer details of the IPR related to Covaxin is debated, how it got to be developed is a saga of scientific research in India.
Inactivated virus vaccine
Covaxin is a class of time tested vaccines known as inactivated whole virion vaccines. It has a good track record of generating long-lasting immunity for many different viral diseases, such as flu, polio, and yellow fever.
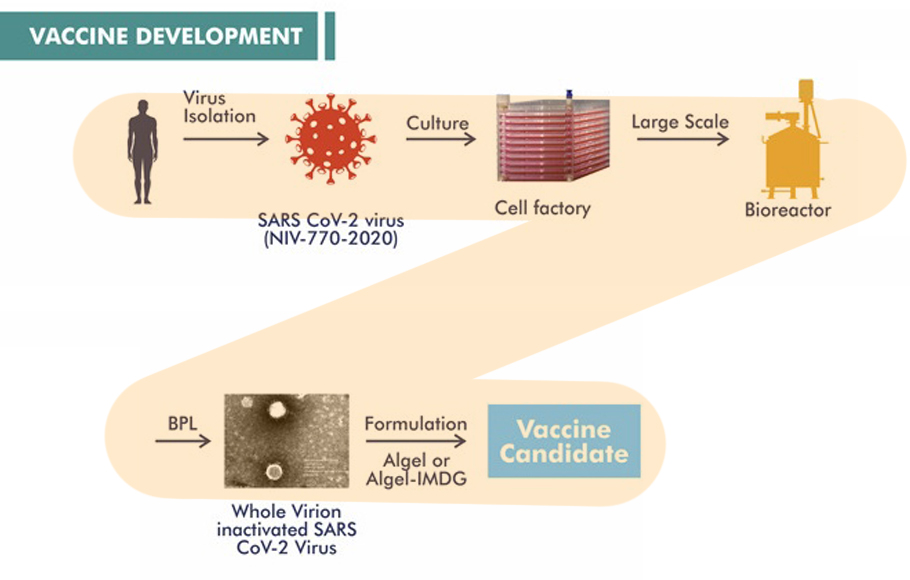
Disease-causing pathogens are cultivated and then inactivated by dousing them with chemicals such as formaldehyde and beta-propiolactone. These chemicals interact with the virus’s genome and make it non-functional while leaving much of its structure intact. In the absence of an active genome, these viruses are ‘biologically inactive’; that is, they cannot infect host cells, reproduce and cause disease.
On the other hand, as their three-dimensional structures are almost untouched, the inactive pathogens can present their ‘antigen’, spatial protein structures, to the immune system.
The mammalian immune system is often, once bitten twice shy. Once the immune system is triggered artificially by the vaccine, the immune reaction is strong and swift to the infection. In vaccinated individuals, the pathogens generally cannot take a foothold and cause disease.
Isolating the whole virus
In developing an inactivated virus vaccine such as Covaxin, the first crucial step is to isolate and cultivate the disease-causing virus in a suitable platform. RT-PCR needs only genome fragments to identify infection. To isolate a whole virus, one needs a well-preserved sample.
When the first three cases of infection were identified in Kerala among the students who returned from Wuhan, ICMR-National Institute of Virology (ICMR-NIV), Pune, collected the samples and tried to isolate the virus. But as the sample quality was not good, they could not succeed.

However, they did not lose heart and kept on trying. Finally, during March 2020, a team of scientists led by Pragya D Yadav, Maximum Containment Laboratory, ICMR-NIV, and Varsha Potdar, Influenza Group, ICMR-NIV, succeeded in isolating a strain of novel coronavirus now named ‘NIV-2020-770’. This virus was isolated from the nasal and throat swabs drawn from a tourist who had arrived in New Delhi with a travel history to Italy.
Till then, only China, Australia, Korea, Germany and the USA had isolated the SARS-CoV-2 virus in the human airway epithelial cells.
Soon the NIV researchers sequenced the genome of NIV-2020-770 isolate and deposited it in the international GISAID repository under the entry EPI_ISL_420545. Further, electron microscope images of this virus were also taken to characterise its physical structure.
NIV-2020-770 isolate virus is part of the “20A” clade of the novel coronavirus family tree. It is identical genome-wise to the earliest strain Wuhan Hu-1. With 19A and 19B branches of family tree wilting, 20A is the founder of the current predominantly circulating lineages worldwide.
This seed virus was given by the NIV institute of ICMR to BBIL for use in the testing and manufacturing of the BBV152 vaccine candidate, commercialised later by BBIL in the name of ‘Covaxin’.
Culturing the virus
A bacteria can be cultured in a petri dish. Once you supply a nutrient medium, the bacteria will happily devour and multiply. However, the virus cannot reproduce on its own. The novel coronavirus infects and hijacks the human cellular machinery to prepare copies of its viral proteins and genome. Once infected, typically, a human cell churns out 1000 copies of the virus in 10 hours. Viruses do not survive much outside their host.
Over the years, scientists have found tricks to cultivate the virus outside of the host using a technology developed by two Japanese scientists, Yasumura and Kawakita, at Chiba University in 1962.
They had isolated epithelial kidney cells from an adult, female African green monkey (Chlorocebus sabaeus) and tried to grow them in a petri dish. Just like the Parsi holy fire never stops burning, these cell cultures fed with nutrients divide untiringly without ever entering senescence, a type of biological ageing found in post-replicative cells.
The original cell line was called Vero. These immortalised Vero cell lines, widespread among biotech research, typically lack interferons, the antiviral signalling proteins naturally produced by mammalian cells.
Hence, Vero cells are susceptible to infection by many viruses, making them prime candidates to cultivate viruses. But they still have the receptors for interferon, so they respond when interferon is added to the culture media. Hence this platform can be used for testing the efficacy of antiviral drugs and vaccines. In addition, Vero cells are frequently used for producing inactivated virus and protein-based vaccines.
After many trials and tribulations, researchers from NIV successfully cultured the NIV-2020-770 isolate on the Vero CCL-81 cells platform. When inoculated with novel coronavirus, as the infection progressed, Vero CCL-81 cells bulged.
As the virus started to multiply, the number of Vero cells increased as much as 26 times. In addition to Vero cells, the scientists were also able to culture the novel coronavirus in the Calu-3 (human airway epithelial cells derived from human bronchial submucosal glands) cell platform, which was needed to do further studies related to vaccine development.
Search for suitable adjuvant
Having cultured the virus in the Vero cell platform, scientists at NIV and BBIL toyed with the idea of developing an inactivated virus vaccine candidate. This was developed and subsequently named BBV152.
Vaccine formulations often contain a substance called an adjuvant, over which the virus is precipitated. Until recently, alum was the most commonly used adjuvant. While precipitation onto alum promotes the uptake of the immunogen, this often initiates relatively more of T-helper cells 2 (Th2) type responses than the T-helper cell 1 (Th1) type response.
The Th1 and Th2 cells play an essential role in immunity. Th1 cells secrete cytokines and induce humoral response producing neutralising antibodies. Th2 cells secrete interferon and induce macrophages, natural killer cells and T cytotoxic cells, and the production of opsonising antibodies by B-cells leading to a cell-mediated response.
The combination of humoral- and cell-mediated responses generated by Th responses is necessary to control intracellular infections., Hence, SARS CoV 2-specific T cell immunity is critical while developing a vaccine against SARS CoV 2.
As the alum adjuvanted vaccines poorly elicit the desired Th1 response, the NIV researchers’ team dealt with this potential concern using a particular adjuvant called IMDG obtained from a company ViroVax USA. This adjuvant is prepared by imidazoquinoline molecules ‘sucked’ onto aluminium hydroxide gel surface by chemical bonds (chemosorbed)
Alum (Algel) is often used as an adjuvant in many vaccines globally and is known to be safe. However, Algel-IMDG is new. To test its safety, the Vero cells with novel coronavirus were fed with Algel-IMDG to see if this drives mutation in the virus genome.
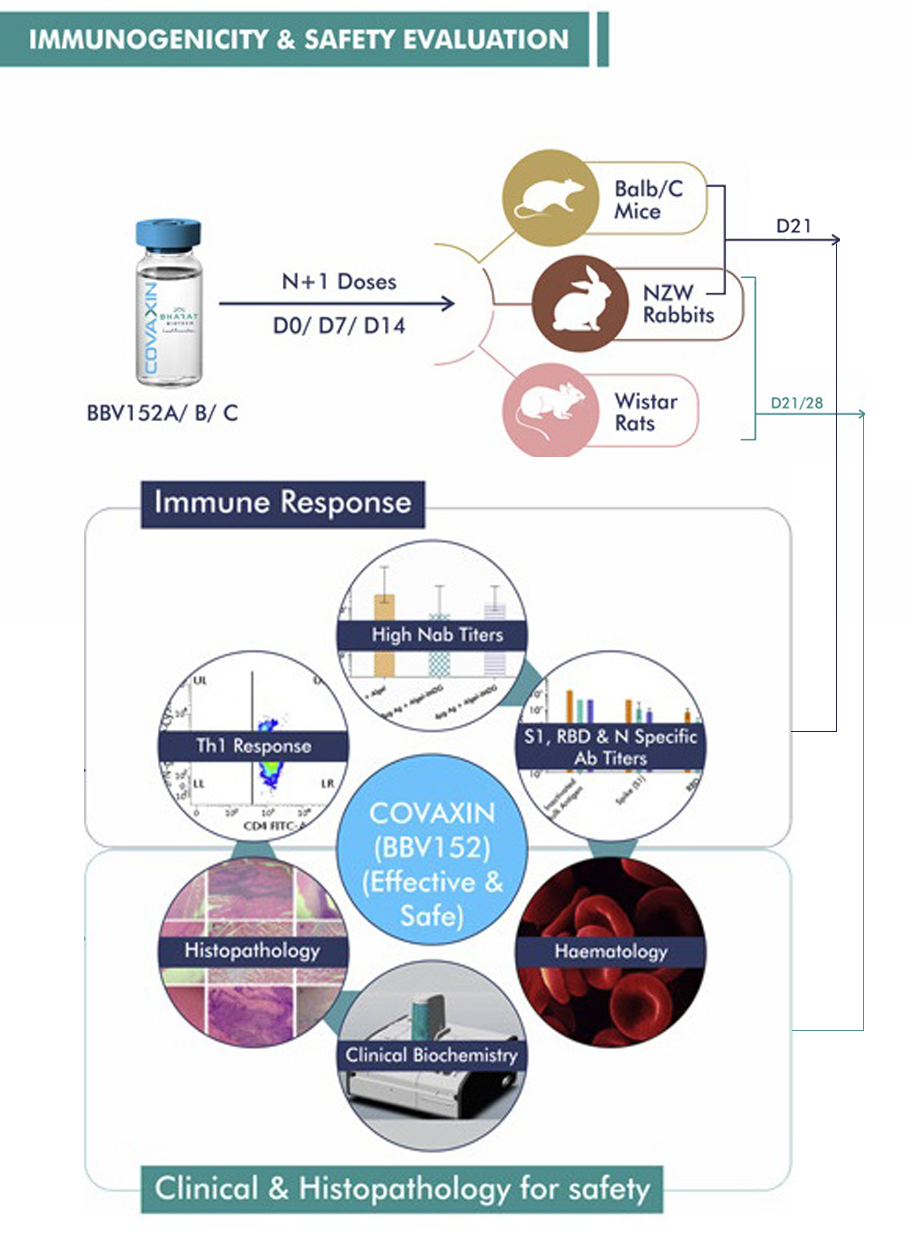
Second, different dosages of Algel-IMDG were given to animals (mice, rats and rabbits) to know the dosage toleration. Third, animals were given multiple dosages to determine if the repeated administration of Algel-IMDG causes any systemic toxicity or mortality.
Further animals administered with antigen (inactivated virus) alone or adjuvant alone or adjuvanted vaccine candidate with inactivated virus formulations were studied. They found none of these formulations caused harm to the animals.
From these, the researchers from NIV, BBIL along with other collaborators from ICMR, RCC Laboratories India Private Limited, Translational Health Science and Technology Institute (THSTI), figured out in these studies funded by ICMR and BBIL the safety and immunogenicity of the vaccine candidate BBV152.
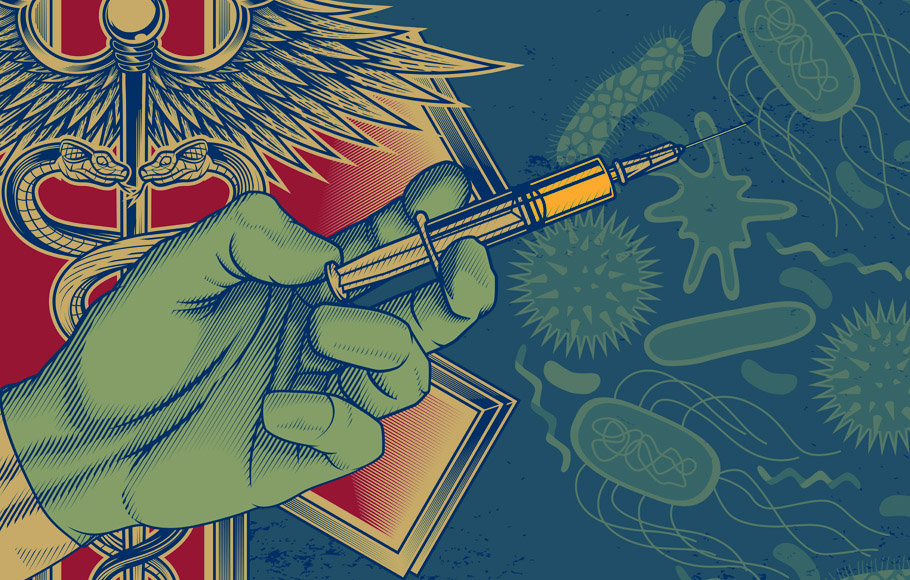
Evaluation in animal model
Vaccine development crucially depends upon ‘animal models’ to test the vaccine’s efficacy. Model animals have biology that mimics various aspects of the disease found in humans when infected with that pathogen. Such model animals are first administered the vaccine candidate and then deliberately exposed to the disease-causing pathogen to see the effect of the candidate vaccine.
In May 2020, a research team led by Masaki Imai, Department of Microbiology and Immunology, Institute of Medical Science, University of Tokyo, found that the Syrian hamsters perform excellently as an animal model for Covid19.
SARS-CoV-2 isolates replicate efficiently in the lungs of Syrian hamsters. Once infected with SARS-CoV-2, the lungs of the hamsters show severe pathological lesions similar to COVID-19 patients with pneumonia.
Infected hamsters develop neutralising antibodies. The plasma serum, rich with these antibodies, when transfused to another hamster, gives passive protection. In short, the hamsters were mimicking human Covid19.
Swiftly, Pragya D Yadav and Sreelekshmy Mohandas of NIV and their team swing into action. They tested along with their collaborators the inactivated virus vaccine candidate BBV152 made from the NIV-2020-770 isolate in the Syrian hamsters.
When vaccinated hamsters were deliberately infected with the virus, the study showed the rapid clearance of the lower respiratory tract. Candidate vaccine reduced virus load in the upper respiratory tract.
Further, the lungs were unaffected. Moreover, the researchers found that the formulation with imidazoquinoline adsorbed on alum adjuvant remarkably generated a quick and robust immune response biased towards Th1. All one wanted for a successful inactivated virus vaccine was there.
Candidate vaccine development
By early 2020, the Covid pandemic had engulfed the entire globe. Countries one after the other were imposing crippling lockdown to control the wildfire. Researchers across the world raced to develop a vaccine. By March 2020, China had developed two inactivated SARS-CoV–2 vaccine candidates that showed promising results in preclinical trials.
ICMR entered into an agreement with Bharat Biotech International Limited (BBIL), Hyderabad, in May 2020 and established the viability of the inactivated vaccine candidate from the seed novel coronavirus and the desirability of Algel-IMDG adjuvant.
BBIL is known for having developed 10 different viral vaccines and has delivered over five billion doses. Culturing, inactivating, and testing was undertaken in the NIV laboratory. BBIL’s biosafety level-3 facility in Hyderabad manufactured industrial samples for animal studies and clinical trials.
Stability and safety of vaccine formulations
Three vaccine formulations were made by NIV and BBIL. The first formulation had 3 micrograms of inactivated virus + Algel-IMDG. The second had 6 micrograms of inactivated virus + Algel-IMDG, and the third 6 micrograms of inactivated virus + Algel.
In addition, they made a formulation that contained just the Algel to serve as a control. These four formulations, named BBV152 A, B, C and D, respectively, were used in animal testing and human clinical trials to establish their relative immunogenicity and protective efficacy.
Vaccines, once manufactured, have to be packed, stored, transported and administered. The vaccine formulation must remain stable for a longer time. Samples of the three formulations were held at 37°C and 2–8°C temperature for 7 days. After seven days, the samples were tested, and it was found that the formulations were stable even at 37°C for seven days.
Further, as mentioned earlier, the safety of adjuvanted vaccine formulations was tested in mice, rats and rabbits. The effect of the full dose, 1/10th dose, and 1/20th dose was studied in these animals.
The studies demonstrated that even with a repeated dose, no mortality occurred. Moreover, the animals in the study showed no changes in clinical signs, body weight gain, body temperature, or feed consumption.
Other than local reaction at the injection site, no other treatment-related microscopic findings were observed in any test, establishing the safety aspect of the vaccine candidates.
Immunogenicity
Along with safety, vaccines need to evoke an immune response. The researchers also compared keeping the gap between the first and second dose seven days and 14 days. One group of mice were given the second dose on the seventh day, and the second group with a 14-day gap.
The spike-protein-specific antibody levels increased eightfold when the gap was 14 days as compared to the seven-day gap. Moreover, the antibody was found in significance even 12 weeks after the last dose, indicating a vaccine-induced long-lasting immune response.
For a vaccine to work in the real world, it must address the natural mutations taking place in the pathogen. The virus mutates, and new variants emerge over time, and the vaccines must elicit an adequate response to them. Bioinformatic analysis of the SARS-COV-2 virus showed that the nucleocapsid protein also has both T and B cell immunodominant epitopes in addition to spike protein.
Further, in comparison to spike protein, researchers found that the nucleocapsid protein undergoes relatively lesser mutation. Hence, if the nucleocapsid protein retains its core shape after inactivation, the vaccine would be effective against most emergent variants, even when the variant has a crucial mutation at the spike protein.
Lab studies showed that the candidate vaccine BBV152 elicits neutralising antibodies against antigens on the spike protein, nucleocapsid protein and the receptor-binding domain on the spike protein.
This indicates perhaps the structural integrity of both spike and N proteins during the inactivation is retained. And that may be one of the key reasons behind the various variants that this vaccine can deal with.
Monkey trails
Once the BBV152 formulation proved effective in small animals, the researchers at NIV and BBIL moved to test its efficacy in rhesus macaques (Macaca mulata).
In this randomised control trials, 20 macaques were divided into four groups. The control group was administered a placebo, a formulation with the adjuvant but not the inactivated virus. The remaining three in the vaccine arm were given BBV152A, BBV152B, and BBV152C formulations.
The second dose of these formulations was given after fourteen days. After 14 days from the second dose, all the animals were put to a challenge test. They were intentionally exposed to novel coronavirus. If a particular vaccine formulation worked, that group must show a higher protective immune response.

Periodically, blood samples were drawn from the macaques and examined for the presence and strength of SARS-CoV-2 specific IgG and neutralising antibodies. Post intentional infection, the viral load was estimated from the bronchoalveolar lavage fluid, nasal swab, throat swab. Lung tissue samples were taken seven days post-infection and studied for lesions.
The study clearly showed no evidence of pneumonia in the vaccinated groups. Whereas, in contrast, the unvaccinated placebo group monkeys showed interstitial pneumonia and severe illness.
Onwards to human trial
The preclinical studies on mice, rats, rabbits, hamsters and macaques provided confidence to go for a human clinical trial. The researchers from ICMR and BBIL tied up with nine medical hospitals to conduct phase 1 clinical trial at 11 centres.
In this double-blind, randomised controlled clinical trial, 375 participants aged between 18 and 55 were randomly assigned to four groups. Three groups of 100 each received two doses of BBV152A, BBV152B, and BBV152C 14 days apart. The fourth group, called the placebo arm, had 75 participants administered a formulation that contained only Algel adjuvant.
Follow-up visits were scheduled on days 7, 14, 28, 42, 104, and 194 after the first dose and blood samples were collected. Any adverse event was recorded.
In December 2020, the results of phase 1 trials were announced. There was no adverse reaction, except for mild events. One serious event was reported and investigated. This event was found to be unrelated to vaccination.
Analysis of the data showed that the seroconversion of the body’s production of virus-neutralising antibodies occurred in 88% of Group A, 92% of Group B and 83% of Group C. However, the BBV152A and BBV152B having Algel-IMDG adjuvant gave good result concerning triggering Th1 response. Therefore, only BBV152A and BBV152B were selected for the phase II clinical trial.
The phase II clinical trial commenced during September 2020 and had 380 participants. 190 of them were administered BBV152A while the other BBV152B. But this time, the gap between the two doses was kept at 28 days apart.
After the study, the results published in March 2021 showed that BBV152B was more effective when given 28 days apart.
BBIL commenced the phase III clinical trial of 26,000 volunteers from across India in November 2020. In April 2021, in its interim analysis of its phase 3 trial, BBIL reported an efficacy of 78%. The final report is awaited.
The vaccine candidate BBV152B is called the vaccine Covaxin.
Meanwhile, in a study conducted in the USA, Covaxin, India’s home-grown COVID-19 vaccine, has been found to neutralise the B.1.617 variant, which is dominant amongst the sequenced samples of the novel coronavirus from the Indian population.