- Home
- News
- Analysis
- States
- Perspective
- Videos
- Education
- Entertainment
- Elections
- World Cup 2023
- Features
- Health
- Budget 2024-25
- Business
- Series
- NEET TANGLE
- Economy Series
- Earth Day
- Kashmir’s Frozen Turbulence
- India@75
- The legend of Ramjanmabhoomi
- Liberalisation@30
- How to tame a dragon
- Celebrating biodiversity
- Farm Matters
- 50 days of solitude
- Bringing Migrants Home
- Budget 2020
- Jharkhand Votes
- The Federal Investigates
- The Federal Impact
- Vanishing Sand
- Gandhi @ 150
- Andhra Today
- Field report
- Operation Gulmarg
- Pandemic @1 Mn in India
- The Federal Year-End
- The Zero Year
- Premium
- Science
- Brand studio
- Home
- NewsNews
- Analysis
- StatesStates
- PerspectivePerspective
- VideosVideos
- Entertainment
- ElectionsElections
- Sports
- Loading...
Sports - Features
- Budget 2024-25
- BusinessBusiness
- Premium
- Loading...
Premium
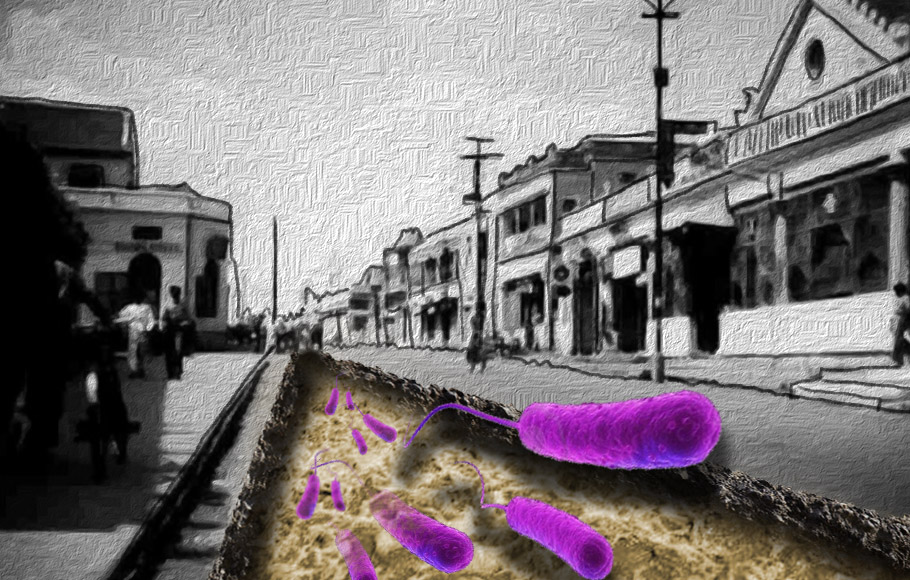
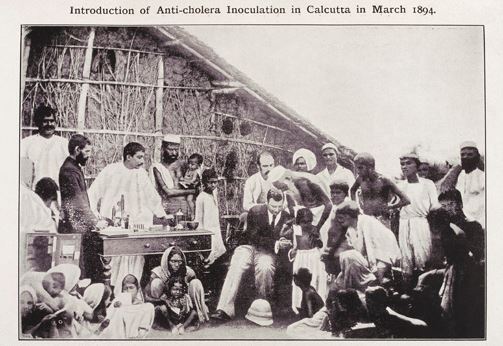
Contact tracing, hotspots and plodding through sewers: Cholera in Bangalore 1895
During the cholera outbreak in Bangalore in 1895, there was then, as now, a constant battle between faith and reason, both in India and the UK.

Epidemics of smallpox, plague and cholera have been part of human history for ever and ever and our partial success over the past few decades has perhaps inured us to the twists and turns of biology and evolution, and thus disease and epidemics. In India, systematic efforts to battle epidemic disease were first attempted in the 19th century, armed with the new knowledge coming out of the works...
Epidemics of smallpox, plague and cholera have been part of human history for ever and ever and our partial success over the past few decades has perhaps inured us to the twists and turns of biology and evolution, and thus disease and epidemics.
In India, systematic efforts to battle epidemic disease were first attempted in the 19th century, armed with the new knowledge coming out of the works of Koch, Virchow, Pasteur, Jenner; the sanitation engineering of Brunel; and the experience of the Indian Medical Service (IMS), supplemented by the increasing numbers of Indians who were actively engaged in the medical professions, at various levels.
There was then, as now, a constant battle between faith and reason, both in India and the UK, and the world of the recently discovered bacteria excited all kinds of apprehensions, much like the even ‘smaller’ viruses provoke ‘shock and awe’ now.
One wry editorial in the Indian Medical Gazette pointed in 1876, as evidence of local superstition, the practice in southern India of beating drums and blowing horns to drive an illness (dengue) out of a village (apparently to the next one!); a process which, they were also quick to also admit, was similar to the faith in miracle cures in Europe.
Bangalore in crisis
One of the officers of the IMS was Ronald Ross, who later won the Nobel Prize for Medicine based on his work on malaria in India. While posted to Bangalore, he was entrusted to make an enquiry into the appalling sanitary conditions in the 1890s, a decade after the British had transferred power back to the local administration. The city had just been though both a famine and the plague, and was understandably in crisis.
The once leafy city, parts of which, especially St Johns Road, ‘resembled an English village’, had become too dirty and was fast losing its ‘salubrious nature’. Since this was a premier Cantonment, its decline was felt to be very significant. The city had been rather carefully built up, after the depredations of the Anglo-Mysore wars of 1793, a century earlier. The city and its surrounding areas had then come to resemble an empty scrubland, more a desert than anything else.
By the middle of the 19th century, however, so many trees had been planted that some officers felt that it now resembled a forest! Since this was also a botanical and medical research station, exotic trees were planted and the city became famous for its green environs and healthy air.
The report by Ronald Ross about the reasons for its decline by the end of the century was thus carried with editorial concern in the Indian Medical Gazette in June 1896. Its comments will sound startlingly contemporary.

Challenges before Ross
A previous Residency Surgeon, Lt Col. Dobson, had earlier expressed great dissatisfaction with the state of Bangalore and suggested remedies, but these were thought impractical and expensive. He had specifically pointed out that the “sanitation of the town was not properly managed, both generally, and with special regard to the treatment of epidemics”. The Resident had shared the concern of the Surgeon, and pointed out that the crisis was ‘probably attributable in part to the defective sanitation’ as well as the ‘absolute ignorance displayed by every member of the department’.
They had tracked the origin of the disease, through contact tracing, down to one person who had come in from Madras, and after affecting people around the house and the lane, the disease had appeared almost a mile away within a week. Testing was not possible as samples had to be sent to Madras, and the laboratory there claimed it did not know how to do this (a matter of surprise to the doctors, as the tests were widely available in Europe at that time).
Problem with private contractors
This report on the cholera epidemic in September 1895 prompted another enquiry, this time by the Surgeon-Major on special duty, Ronald Ross. He blamed the sorry state of Bangalore to the fact that the conservancy (sanitation and waste disposal) of the native (Indian) quarters was handed over to private contractors, with totally unsatisfactory consequences. This had been done in 1884, soon after the British administration left, with less than happy result; as the contractors “remove filth at their convenience…collections of many days”; and that the “inhabitants live in and amongst their own excreta”. The source of fresh water supply was so contaminated that the Millers’ tank No. 4 had 6,00,000 bacteria/cubic inch.
This was an early failed experience with privatisation that continues to repeat itself. The regularity with which the same service is found to be lacking, and yet new private contractors are invited, is quite illuminating of our reluctance to learn from experience. Also illustrative is Ross’s dismissal of the role or importance of privatisation, a tension between private enterprise and public service that clearly continues till date.
Although the usual excuse of a fund crunch was offered in 1896, Sir Ronald Ross was skeptical about this. The editors of the Gazette had agreed that while spending, ‘the funds were not utilised to the best advantage’, and at the same time, ‘sources of income were not properly developed’. Of course, Ross had also produced a document that showed that proper management and conversion of waste, could actually return a modest profit, thus, emphasising the short-sightedness of government spending, that calculated price, but was ignorant of the value of the service. Private profit and good public services were not thought compatible then, and one wonders if they are now.
When sanitation ran against gravity
Ross observed that the drains that ran through Blackpully (now Shivaji Nagar) were ill maintained, and indeed were ‘opposed to all sanitary rules and principles’ and often “ran against gravity”! Cholera was endemic in this densely populated area (50,000 in 1.5 square miles), and most cases occurred along the sides of the open sewer that ran through it.
Dr Ross’ brief was to investigate this and suggest improvements, using his knowledge of bacteriology, which then, was only a few decades old. He commented that “It was at once apparent that the latrines throughout the town were of most ineffective kind, while carting being given over to native contractors, to the misreading of Municipal Regulations, and to the state of the latrines and other causes, conservancy was in a very evil plight. It was apparent, moreover, that the drains throughout the station (Bangalore) were constructed on an entirely wrong pattern, latrines were built on old lines, there were only four public urinals, the sale of water, milk and aerated drinks was not regulated…in short, sanitation was in so embryonic a condition that the only idea which seems to have suggested itself, or to have been acted upon, was that it is necessary to place a gutter by the side of every street, and to provide a few sewers.”
The accounts by Ross are quite detailed. He personally inspects a number of households, takes stool samples from toilets, as well as water pumps, milk, food stalls etc. Often, the cases were not notified at all, and he pointed out that “locking up the house and disinfection after the spread had already occurred was not likely to be useful”! Disinfection of all belongings, and cleanliness was ordered, as was destruction of many personal items thought to be infected (but only after due compensation).
It was urged that all residents be provided pails or pots for collecting night soil. Surprisingly, the garden houses (bungalows) had extensive sewage, but were not charged for the service while the ‘natives’ lived without any sewage at all. Case maps were produced every day, documenting the geographical spread to various corners of the station.
In the absence of enough water, and expense, the best that could be suggested was a good ‘dry-conservancy system’. A microscope was urgently ordered, and this helped estimate the extent of infection much better, but the citizens baulked at the idea of getting inoculated!
Ross was able to convince only one person among the relatives of someone who had been infected to take a dose of the new vaccine from Haffkine in Bombay. He was also at pains to point out that the health of the officers of the Cantonment was subject to the same risks as that of the natives.
His mantra of disinfecting anything and everything proved successful, and the number of infected declined from 13 cases in the week of September 10, down to 2 cases in the week of October 13. In all, there were 35 cases and 25 deaths, during the four weeks that Ross observed the epidemic and worked.
In his concluding remarks, he lays emphasis on the fact that surface water and sub-soil water (wells) in Bangalore could not be trusted, and it was perhaps best to disinfect them all at regular intervals. Of course, now that most of the city still relies on the same old wells, only deeper, is a great achievement.
The Municipality had no ‘machinery’ (method) of dealing with epidemics, since the medical authorities were devoid of any power or opinion to influence the administration. He thus suggested an elaborate administrative machinery to look after public health and vaccination, costing 60,000 a year in salaries, but also pointed out that reasonable charges, and sale of night-soil would earn 80,000 per year.
The Administration, probably irked by these criticisms, and the extra costs and headache, shunted Ross off to Coonoor, the experience leaving him mentally exhausted, as he said in a letter, “I have just finished the report on the sanitation of Bangalore which has reduced my brain to a pulp”.
In Coonoor, according to a recent biography, a local tribal showed him the mosquito that was responsible for the spread of malaria, paving the way for the award of the Nobel Prize to Sir Ronald Ross! So even the clouds of administrative intrigue have a silver lining.
It would be interesting to explore whether any of the recommendations were carried out in the intervening 125 odd years. Less than 40 deaths in a small town of Bangalore (pop. 100,000) in a Native Kingdom were enough to warrant concern all the way to Calcutta and London, and provoke widespread change.

Of course, a Public Health Department was created in every Municipality, but the advice that a medical person head it was forgotten over time, especially after the disbanding of the Indian Medical Service itself after Independence. After all, to expect allegiance to Virchow’s statement that ‘politics is nothing but medicine at a larger scale’ by politicians who had spent some decades deciding on how to partition the country on religious or linguistic lines was hardly to be expected.
Given the consistency of these problems, it seems likely that none of these criticisms, keeping the advances in our understanding of how diseases occur and spread, were taken seriously. Not much seems to have changed, except that the gutters themselves have been removed, to allow the rain to turn roads into streams, in which water flows towards the memory of long dead lakes.
The green belts, which provided a natural ecological barrier between dense habitations have disappeared too. Pure water, to drink or to wash with, remains a distant dream in a country blessed with an entire season of the monsoon. We produce several billion litres of extra neutral alcohol (96% alcohol), but struggle to provide enough disinfectant alcohol (70%) for sanitisers while potable alcohol (40%) is aplenty.
Having been the first to have a Medical College east of the Suez and a long history of organised medical services, and the largest single producer of medical graduates in the world, we find no anachronism in importing testing kits and equipment and technology from countries that were once far behind us.
And sanitation, and cleanliness, is still something to be aspired to, and minuscule bits of single stranded RNA have the capacity to tie the whole of humanity into knots!
(Sanjeev Jain is Professor, Department of Psychiatry, National Institute of Mental Health and Neuro-Sciences (NIMHANS), Bengaluru and Alok Sarin is a psychiatrist at the Sitaram Bhartia Institute, New Delhi)