
- Home
- News
- Analysis
- States
- Perspective
- Videos
- Education
- Entertainment
- Elections
- World Cup 2023
- Features
- Health
- Business
- Series
- Economy Series
- Earth Day
- Kashmir’s Frozen Turbulence
- India@75
- The legend of Ramjanmabhoomi
- Liberalisation@30
- How to tame a dragon
- Celebrating biodiversity
- Farm Matters
- 50 days of solitude
- Bringing Migrants Home
- Budget 2020
- Jharkhand Votes
- The Federal Investigates
- The Federal Impact
- Vanishing Sand
- Gandhi @ 150
- Andhra Today
- Field report
- Operation Gulmarg
- Pandemic @1 Mn in India
- The Federal Year-End
- The Zero Year
- Premium
- Science
- Brand studio
- Home
- NewsNews
- Analysis
- StatesStates
- PerspectivePerspective
- VideosVideos
- Entertainment
- ElectionsElections
- Sports
- Loading...
Sports - Features
- BusinessBusiness
- Premium
- Loading...
Premium
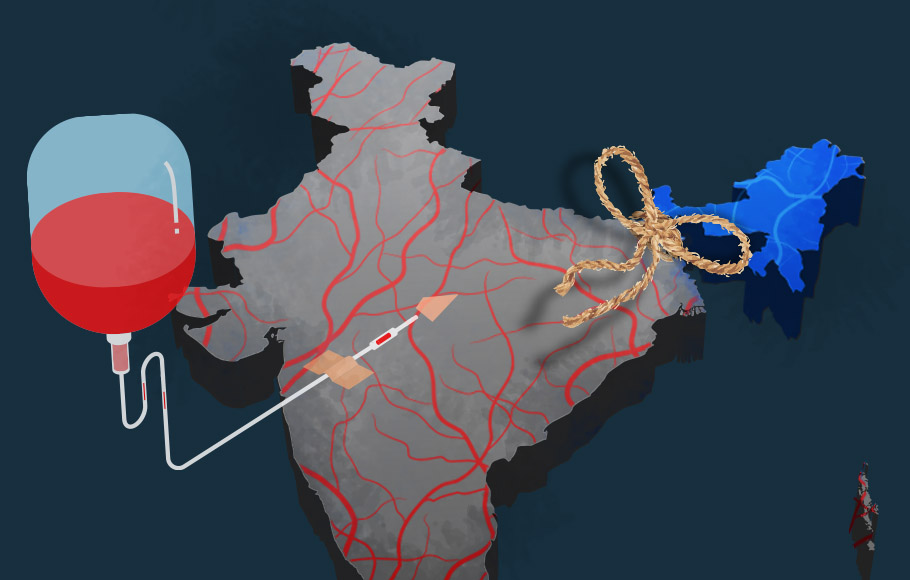
Arunachal gets its first ICU as Covid-19 exposes NE's health woes
Apart from Assam, most of the northeastern states have poor healthcare infrastructure, that leaves them exposed in the battle against COVID-19.

Within hours of detecting the first COVID-19 case in his state on April 2, Arunachal Pradesh chief minister Pema Khandu dialled up his Assam counterpart Sarbananda Sonowal. Khandu wanted Sonowal to help accommodate critical patients from his state in medical facilities at Assam’s Dibrugarh or Guwahati. The pre-emptive request was inevitable considering the Himalayan state, which...
Within hours of detecting the first COVID-19 case in his state on April 2, Arunachal Pradesh chief minister Pema Khandu dialled up his Assam counterpart Sarbananda Sonowal. Khandu wanted Sonowal to help accommodate critical patients from his state in medical facilities at Assam’s Dibrugarh or Guwahati.
The pre-emptive request was inevitable considering the Himalayan state, which attained statehood in February 1987, had its first ever intensive care unit (ICU) opened only about a week before at the Tomo Riba Institute of Health and Medical Science (TRIHMS), the state’s first medical college inaugurated two years ago at Naharlagun near Itanagar.
Around the same time when the chief minister was on the phone discussing the future course of action, officials from Arunachal’s Upper Dibang Valley district during a feedback survey told the Prime Minister’s Office that the closest testing centre was 379 km away, at Dibrugarh (Assam), which made sample collection and testing time-consuming and arduous.
State health minister Alo Libang was candid enough to admit that the health infrastructure was getting due attention only after the outbreak of the pandemic.
“We have this habit of running to the doctor only when the ailment gets critical. Similarly, we are realising the importance of health infrastructure after being hit by a pandemic,” he told The Federal over the phone.
The budgetary allocation for the health and family welfare department, the minister said, has been marginally increased in the current financial year.
Major allocations in the health sector in this year’s budget were ₹40 crore for the improvement of infrastructure of the TRIHMS, ₹25 crore for procurement of advanced diagnostic tools for the medical college and hospital and other tertiary hospitals, and another ₹24 crore for upgradation of five hospitals in the districts.
With limited resources, the health department scurried to put up some credible infrastructure to fight the viral enemy.

“We had no ICU facility in the entire state. In the run-up to the coronavirus outbreak, we created a four-bedded ICU at TRIHMS. A similar facility has been introduced in seven district hospitals each and we are in the process of introducing ICUs in 10 more district hospitals. We have also procured 25 ventilators and plan to get more,” Libang said.
Apart from the 500-bed TRIHMS, the state has 21 district hospitals (Arunachal Pradesh has 25 districts in total), 79 community health centres, 169 primary health centres and 588 sub-centres catering to the health requirements of the state’s over 1.68 million people, with a population density of 17 persons per square kilometre.
Itanagar-based 221-bedded Ramkrishna Mission Hospital, started in 1979, is the only major private health facility in the state.
Territorial battle over COVID-19 patient
Arunachal Pradesh is not the only laggard state in the region when it comes to health infrastructure. Participating in the PMO’s feedback survey on COVID-19 preparedness, officials from Nagaland informed that the state did not have a single testing centre.
The absence of a testing facility created a strange case wherein the lone COVID-19 patient from Nagaland found himself unaccounted for. The swab sample of the 33-year-old, a native of Dimapur, Nagaland’s commercial capital, was sent for testing to the Gauhati Medical College and Hospital (GMCH), some 292 km away in Assam. He was tested positive and underwent treatment at the GMCH since April 12.
Now, since the patient was found positive for COVID-19 in the test done in Guwahati, the Nagaland government did not count him as one of its cases. The patient did not either figure in the list of positive cases in Assam as his case was referred to the state.
This attempt to keep a clean slate by the Nagaland government, however, could not hide the state’s poor preparedness to fight the pandemic. The state, as on April 27, has tested only 613 samples.
In its government-run hospitals, there are just 37 ICU beds, which have been now dedicated for COVID-19 patients, and 20 ventilators. Only 18 doctors have received training on use of these ventilators and are assigned to ICU beds, according to a report submitted by Nagaland principal secretary, health and family welfare department, Menukhol John, to the Union health ministry on April 18.
Meghalaya has just 25 beds with ventilators and another 14 can be made available at North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences (NEIGRIHMS), according to health department statistics.
The state has a capacity to test 180 samples per day at the NEIGHRIHMS. Rest of the samples are sent to either Guwahati or Barpeta in Assam.
Other than Gauhati Medical College and Hospital, the Assam Medical College, Dibrugarh (oldest medical college in the region), the NEIGRIHMS and the Regional Institute of Medical Sciences, Imphal, there are not many premier medical institutes in the region.
Even the basic healthcare facilities call for an immediate revamping. At a health summit held in Guwahati last year, it was observed that the availability of community health centres fell short by 50% in Sikkim, 37% in Assam and 17% in Tripura.
The health services in the region are primarily under the government sector, with only a few premier private institutions functioning in Guwahati and Shillong, the two major cities of the region.
Health spending and other shortcomings
The Regional Plan (2017-18 to 2019-20) of the North Eastern Council pointed out that of the eight states in the region, Assam spent the highest (2.1% of SGDP) on health while the other states’ expenditure ranged between 0.3% (Sikkim) and 0.6% (Meghalaya).
Due to the lack of proper health facilities, people from the Northeast spend around ₹120 crore annually outside the region for medical treatment, the NEC observed.
A healthcare summit organised in Guwahati a couple of years ago pointed out that more than 8 lakh additional hospital beds were required in the region.
The shortage of doctors is another area of concern. “Northeast India has a supply gap of 36,009 registered doctors. Also, there is a 66% gap in the supply of trained nurses. There is 1 nurse per 1,483 people which is higher than the national average of 890 and it does not meet the WHO prescribed norms of 3 nurses per 1000 people,” according to a research paper published by the Observer Research Foundation last month.

The NEC, a statutory regional planning body, stressed the need for setting up of more medical colleges in the region to increase the number of doctors.
According to the same research paper, a major hurdle for setting up of medical colleges in the region is that sufficient number of qualified doctors may not be readily available for appointment as professors, associate professors and assistant professors.
As per the Medical Council of India’s guidelines, to become even an assistant professor, one has to publish at least four research papers in national and/or international journals. As India has only a handful of medical journals, it is difficult for the doctors of NE region to publish so many research papers, the ORF paper concluded.
However, health expert Dr Nandira Changkija claims the scenario is improving. Changkija, a former principal director of health and family welfare department of Nagaland, said a “political will” is essential for further improvement.
People should also clamour for their right to have better healthcare facilities, she said.
The best not good enough
Government hospitals even in Assam, which has relatively better infrastructure, make do with around 44% of total requirement of doctors and health officers, according to statistics provided by the Assam State Medical Association last year. The state has one doctor for 1,800 patients.
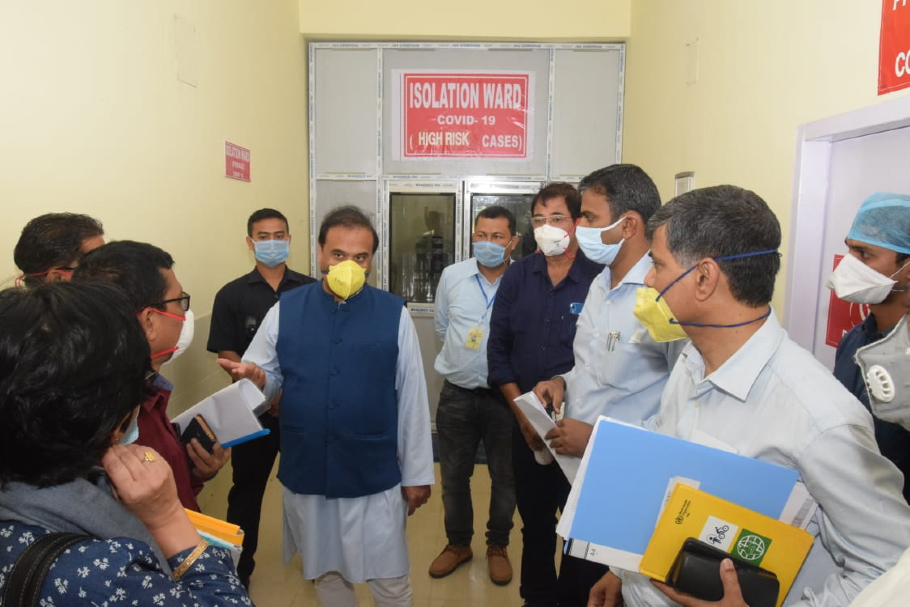
“I have to admit that our health infrastructure is not very strong,” Assam health minister Himanta Biswa Sarma said in a statement on March 24.
According to the Assam health department, there are 440 ICU beds and 303 ventilators in government and private hospitals for treating COVID-19 positive cases.
Inaccessibility a boon or bane?
“The region’s mountainous topography often adds to the problem and makes access to healthcare facilities difficult… Commuting in the region is often time-consuming and cumbersome. With the lockdown in place now, many fear travelling to bigger towns to access critical medical treatment will now become even more difficult,” the ORF’s research paper observed.
Ironically, it is this inaccessibility, which many believe, ultimately proved to be an effective shield for the landlocked region against COVID-19.
Four of the eight clustered states — Arunachal Pradesh, Manipur, Sikkim and Tripura — are now coronavirus-free. Mizoram has one case while the one from Nagaland has recovered.
Most cases in the region are from two relatively more accessible states — Assam (38) and Meghalaya (12).

“Insulation from the outside world, less density of population, apart from stricter adherence to the lockdown rules by the locals helped us contain the disease,” said Libang.
But therein lies the big worry. What will happen once the lockdown is lifted and those from the region stranded in various parts of the country return home? This is one fear that is keeping the region on tenterhooks.
Around 4.26 lakh people from Assam, over 5,500 people from Mizoram and 2,192 from Meghalaya are stranded in different parts of the country, according to the figures provided by the respective state governments.
Although the figures from the rest of the NE states could not be ascertained immediately, it is believed that a sizeable number of people from Arunachal Pradesh, Nagaland, Sikkim, Manipur and Tripura too are stuck outside the region.
Many others are worried that the approaching flood season (that usually starts from early June to October) will further cut off the region from the “mainland”.
To add to the woes of those stuck outside the region, language and cultural barriers have already made the battle against coronavirus more difficult than for the rest of the Indians.
A latest example of this was Mizoram Chief Minister Zoramthanga. Following the PM’s video-conference with CMs on April 27 to plan ahead for COVID-19, Zoramthanga found himself grappling to understand what the rest of the people were talking about. The Indian Express reported that the CM said he did not understand a word of what anyone said. “They were all speaking in Hindi. And I don’t understand a word of Hindi.”

