
- Home
- News
- Analysis
- States
- Perspective
- Videos
- Education
- Entertainment
- Elections
- World Cup 2023
- Features
- Health
- Budget 2024-25
- Business
- Series
- NEET TANGLE
- Economy Series
- Earth Day
- Kashmir’s Frozen Turbulence
- India@75
- The legend of Ramjanmabhoomi
- Liberalisation@30
- How to tame a dragon
- Celebrating biodiversity
- Farm Matters
- 50 days of solitude
- Bringing Migrants Home
- Budget 2020
- Jharkhand Votes
- The Federal Investigates
- The Federal Impact
- Vanishing Sand
- Gandhi @ 150
- Andhra Today
- Field report
- Operation Gulmarg
- Pandemic @1 Mn in India
- The Federal Year-End
- The Zero Year
- Premium
- Science
- Brand studio
- Home
- NewsNews
- Analysis
- StatesStates
- PerspectivePerspective
- VideosVideos
- Entertainment
- ElectionsElections
- Sports
- Loading...
Sports - Features
- Budget 2024-25
- BusinessBusiness
- Premium
- Loading...
Premium

'A political murder, total chaos': Doctors describe India's Covid hell
As people thronged hospitals with Covid-19, oxygen shortage and disruption in supply emerged as a new issue, and doctors had to run after everything.

At midnight on April 23, Dr Pankaj Solanki, a general surgeon running a 50-bedded hospital in Rohini, Delhi, had a nightmare. By then he had worked 42 hours continuously without sleep and his team of health professionals was running around for oxygen. Solanki’s hospital, Dharamveer Solanki Multispeciality Hospital, had 10 ICU beds dedicated for COVID-19 patients, and he could not manage...
At midnight on April 23, Dr Pankaj Solanki, a general surgeon running a 50-bedded hospital in Rohini, Delhi, had a nightmare. By then he had worked 42 hours continuously without sleep and his team of health professionals was running around for oxygen.
Solanki’s hospital, Dharamveer Solanki Multispeciality Hospital, had 10 ICU beds dedicated for COVID-19 patients, and he could not manage without oxygen supply. His patients on oxygen support included a 30-year-old working professional, a pregnant woman, and another patient having a two-year-old daughter.
Two weeks earlier, when the hospital started to receive about 500-600 calls daily seeking hospital beds, Solanki knew things were going to get worse. He had informed his regular suppliers of the situation and they too were aware things would turn ugly soon.
When the crisis struck, the suppliers left him high and dry. And many staff did not turn up for work fearing contraction of Covid-19. Solanki found himself managing the oxygen supply, treating patients, handling calls from anxious attendees of patients, caring for his infected staff and himself—unable to sleep for 42 hours straight.
It was too much for a doctor on duty to handle.
“Running a hospital for nearly 2.5 years, I have never visited an oxygen refilling center till now. But suddenly we were standing in a queue for 12 hours waiting to refill oxygen cylinders,” Solanki says.
His hospital had the capacity to store 1.7 lakh litres of oxygen in 25 cylinders. But after he got whatever he could after spending half a day in a queue, Solanki knew it would not last more than 8-10 hours and he would again have to run around for the next lot. “I did not opt for this,” Solanki tweeted expressing helplessness and the sad state of affairs in the capital city.
“I have seen an eight-year-old standing in line to save his father, an 85-year-old elderly woman to save her husband. People were left to fend for themselves,” he says.
42 hours no sleep coz of #OxygenCrisis. It took us 12 hours to get into filling station,the supplies we have now is till 8 am. Every time have to rush personally to get #oxygen for my patients at @HospitalSolanki
I didn't opt for this.@Asthasaxena88@kaunain_s@thewire_in— Dr Pankaj Dharamveer Solanki (@drpankajsolanki) April 22, 2021
Around this time, the leaders of the ruling BJP, including Prime Minister Narendra Modi and Home Minister Amit Shah, had hopped from state to state campaigning for assembly elections even as Covid-19 cases spiked. As people thronged hospitals, oxygen shortage and disruption in supply emerged as a new issue, especially in Delhi. Soon, the coronavirus started claiming lives so rapidly that crematoriums were seen running full-time.
First wave to the second
Solanki had faced several issues ever since his hospital declared itself open for COVID-19 patients. While financial issues surged on one side, staff shortage hit them on another side. Last year, he had about 27 healthcare workers. During the first wave, the receptionist, security guards and the laundry services stopped. Solanki played the role of a medical director, receptionist, and monitored the security cameras in the hospital.
“Though there was no oxygen crisis or Remdesivir shortage, the first wave had its own difficulties. Back then we were scared. Some were brave enough to go to ICU. We had a difficult time understanding the disease and educating staff about the safety norms,” he says. “We thought that was the worst.”
By the time the second wave happened, he had expanded his hospital and had about 70 staff members. But as soon as the crisis worsened, Solanki worked with barely 50-60% of his staff as some got infected and some left uninformed. He also lost two of his trained ICU specialists who took up another job. “I had no time to run around them. I had to focus on patients,” he says.
We healthworkers are already overworked and underpaid and working in inhuman situations, we were not trained for this, 10 years into the profession so please everyone we are doing the best we can @mithu_jain @drjerrylbanait https://t.co/8ida17EzY9
— Dr.Arushi (@DrArushiJain) May 8, 2021
Only on May 4, the government realised that the shortage of healthcare professionals was yet another concern. It then decided to deploy medical interns.
“The services of final year MBBS students can be utilized for providing services like teleconsultation and monitoring of mild Covid cases after due orientation by and under the supervision of faculty,” Prime Minister announced. “The services of final year PG students as residents may continue to be utilised until fresh batches of PG Students have joined,” he added.
The government also promised to give priority to them in government recruitments after they complete a minimum of 100 days of Covid duty.
Beginning of breakdown
For Solanki, while some patients got discharged, some took transfers to bigger hospitals. Like him, several hospitals in the city started to offload patients on ventilator patients and those who required uninterrupted oxygen supply. Fearing an oxygen shortage, many hospitals stopped new admissions.
As the waiting time tripled, the oxygen supply also delayed. From a six-hour wait time, it increased to 24 hours and then 36 hours on some days.
“The government took control of the oxygen distribution business. But they failed to take control of the network. Suddenly, hospitals were made to stand in line and beg for oxygen,” he says. “It’s a complete mismanagement of administration.”
On April 24, Solanki had to face yet another problem. An angry attendant of one of the patients turned against the management. “A lady barged into the ICU section and tried to take control of the oxygen supply and started to say only her mother will get the oxygen and nobody else will,” he said.
A stressed Solanki had to call the local police and spend 2.5 hours in getting the woman out and transferring the patient to another hospital.
At some point around April 25, Solanki says he felt burnout and wanted to shut down his hospital. “We felt helpless. If the system was in place, we could have and even now can save more people. But the administration did not bother at all,” he said.
Solanki, who’s extremely stressed, says it is very hard for him to destress. Though people advise him to do meditation and do yoga, he says he barely finds time for all that. With less interaction with his own family members, it’s even more painful to handle himself.
“When we get home, we take shower and the food will be kept out on the table. We eat, sleep and ensure the room is locked so that even by mistake the kid does not enter the room and risk infection,” Solanki said. “We cannot devote time for the family either.”
His only interactions with his five-year-old son are through video conferencing.
Solanki says while he did critical non-COVID surgeries last year, he stopped them this year fearing he would get infected.
“Looking at the mortality rate among surgeons, I am scared. We are not superhumans. We have families too to think and care about,” he adds.
Destress apparatus
Even on a normal day, the stress on a healthcare professional is tremendous considering their hectic schedule. The pandemic only worsened it for many.
The situation in bigger Institutions like All India Institute of Medical Sciences, New Delhi, may somewhat be better for doctors as they are placed on fragmented duty on a cyclical shift basis so that they get enough rest.
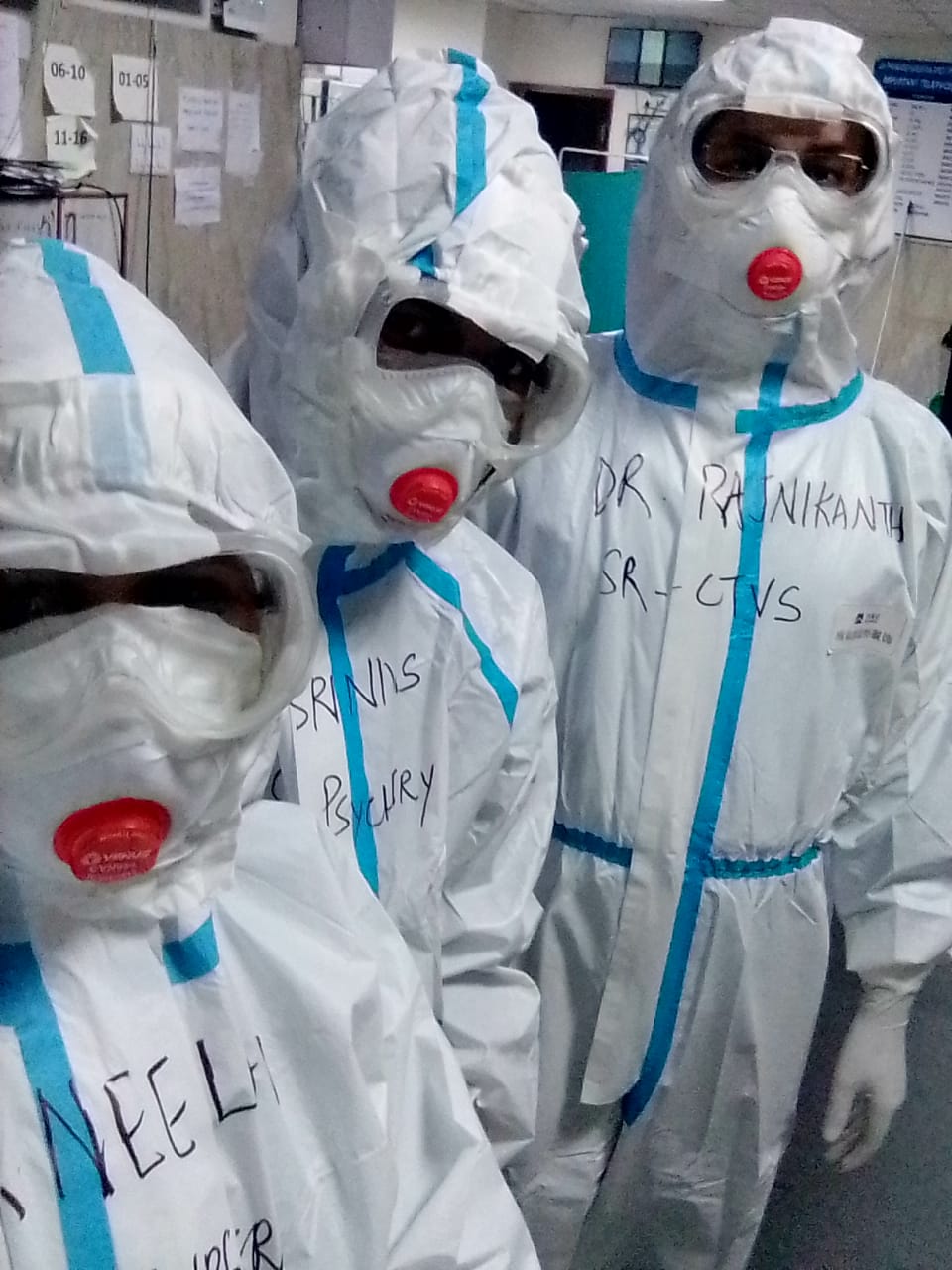
Dr. Srinivas Rajkumar, 33, a consultant psychiatrist and ex-general secretary of resident doctors’ association at AIIMS in New Delhi says to address the mental health issues the institution set up separate helpline for doctors and also the student wellness section introduced programmes like yoga, meditation, an art centre, platform for people to share their anxieties and experience, besides giving psychiatric and counseling help.
He says currently there are calls ranging from simple anxiety symptoms to sleeplessness and post-COVID fatigue.
“Considering suicidal cases in the past within the campus, there are programmes in place for early identification and addressal of mental health issues among doctors,” Rajkumar says. “If you cannot take care of yourself, how will you be able to take care of the patient? So, it’s important to destress,” he adds.
Rajkumar further says it’s difficult for doctors to differentiate between COVID-related fatigue and workplace-related fatigue even as they constantly fear if they are infected, which all adds to the stress.
“It’s just a matter of time before everybody gets infected. By now, 40-50% of the staff at AIIMS would have been infected with COVID since the start of the pandemic,” he says.

In the first wave, Rajkumar says it was all about the quality of PPEs, masks, and other safety kits, and the fear of unknown aspects of the virus. And they somehow tackled it.
But in the second wave, things took a drastic turn. Helplessness and lack of resources hindered their work despite knowing how to handle the virus and infection.
What was worse was that the Parliamentary Standing Committee on Health and Family Welfare had in November last year flagged the issue of inadequate supply of oxygen and asked the government to step up and act back in November 2020. Back then Union Health Minister Harsh Vardhan was busy promoting Patanjali’s unscientific ayurvedic tablet Coronil as a medicine for Covid-19.
Despite expert warnings about the second wave, the government went ahead with elections and made unscientific claims, and strong leaders including Prime Minister Modi went about campaigning without masks.
Despite knowing that a person can be infected when aerosols or droplets containing the virus are inhaled, the cloth masks are said to be not protective, Modi went on to address people wearing a gamcha (a towel), sending a wrong message to people.
“Mistakes happen. Doctors correct it every day. For instance, when a medication does not work or has side effects, we recommend alternative medicines once we gain more patients’ data. In the same manner, why can’t the political leaders admit their mistakes and make course corrections?” Rajkumar asks. “What they have committed is nothing short of a political murder.”
Beyond lack of resources and the thousands of cases and deaths, Rajkumar’s greatest problem even now is the spread of misinformation and false beliefs that everything is under control and everything will be fine.

