
- Home
- India
- World
- Premium
- THE FEDERAL SPECIAL
- Analysis
- States
- Perspective
- Videos
- Sports
- Education
- Entertainment
- Elections
- Features
- Health
- Business
- Series
- In memoriam: Sheikh Mujibur Rahman
- Bishnoi's Men
- NEET TANGLE
- Economy Series
- Earth Day
- Kashmir’s Frozen Turbulence
- India@75
- The legend of Ramjanmabhoomi
- Liberalisation@30
- How to tame a dragon
- Celebrating biodiversity
- Farm Matters
- 50 days of solitude
- Bringing Migrants Home
- Budget 2020
- Jharkhand Votes
- The Federal Investigates
- The Federal Impact
- Vanishing Sand
- Gandhi @ 150
- Andhra Today
- Field report
- Operation Gulmarg
- Pandemic @1 Mn in India
- The Federal Year-End
- The Zero Year
- Science
- Brand studio
- Newsletter
- Elections 2024
- Events
- Home
- IndiaIndia
- World
- Analysis
- StatesStates
- PerspectivePerspective
- VideosVideos
- Sports
- Education
- Entertainment
- ElectionsElections
- Features
- Health
- BusinessBusiness
- Premium
- Loading...
Premium - Events
Coronavirus using a second door to infect human cells. What it means
Another protein receptor called Neuropilin-1 found in the cell walls of blood vessels could be facilitating an alternative gateway for coronavirus.

From smallpox and plague to tuberculosis and the common cold, the first hurdle in controlling an infectious disease is finding out how the virus or the bacteria that causes these illnesses actually enter the human body. Scientists researching the SARS-COV-2 virus – the novel coronavirus that causes Covid-19 – crossed that hurdle several months ago. Or so they thought. Early...
From smallpox and plague to tuberculosis and the common cold, the first hurdle in controlling an infectious disease is finding out how the virus or the bacteria that causes these illnesses actually enter the human body. Scientists researching the SARS-COV-2 virus – the novel coronavirus that causes Covid-19 – crossed that hurdle several months ago. Or so they thought.
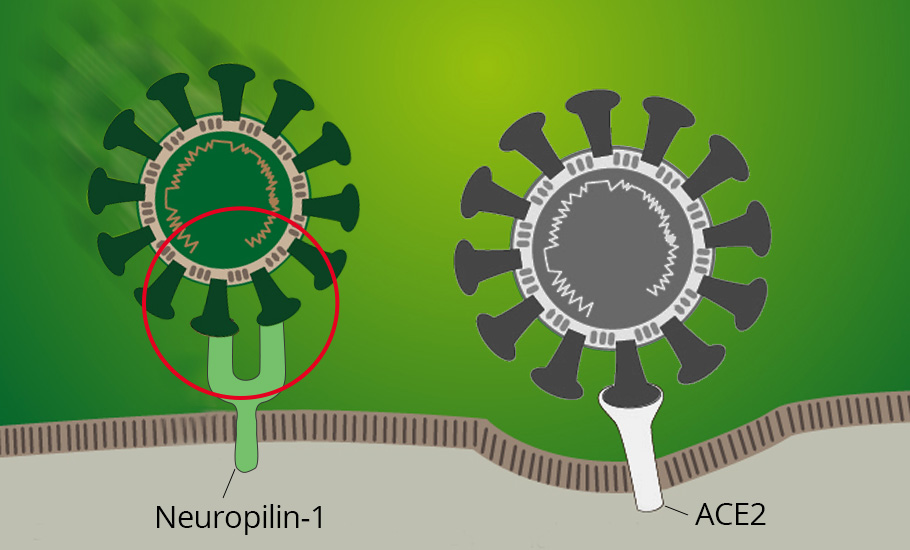
Early investigations showed that SARS-CoV-2 infects human cells via a receptor protein called ACE2. But two international teams of researchers now reveal that the coronavirus could be finding other entryways independent of the ACE2 receptor. Their results published in the journal Science indicate that another receptor called Neuropilin-1 could be facilitating an alternative gateway for the virus. Neuropilin -1 is found in the cell wall of several tissues in the human body.
The chosen one
Viruses cannot multiply by themselves and hence invade other living cells to replicate. The virus-host attachment phase is a key stage in the viral life cycle. For this, viruses single out cell types by utilising proteins as hooks. However, the viral protein cannot latch with all kinds of host cells. For example, HIV infects certain types of white blood cells, and the SARS Cov 2 is known to attack the cells lining airways in the lungs.
Their usual modus operandi is to look for potential proteins called receptors that structurally match their hooking proteins, similar to a lock-and-key mechanism. When there is a match, a gateway opens in the host cell wall through which the virus gains entry to the cell interior. After which, the virus hijacks the cell’s machinery and makes several copies of itself. The surge of viral particles overwhelms the host cell bursting open its cell wall, releasing the viral particles. The process continues with the viral load attacking neighboring cells, thereby causing infection in the host body.
The coronavirus operates similarly. However, preliminary research had only revealed that the virus uses a so-called spike protein to bind with the ACE2 receptor protein to enter the human body.
The stealth mode
Viruses can invade particular cells or multiple cell types, or a range of tissues in organs. This feature is called ‘tissue tropism’ and is governed by several factors involving the pathogen-host interactions. For instance, the influenza virus attacks cells in the upper respiratory tract. In contrast, some types of bird flu viruses are highly virulent on the lower respiratory tract tissues.
The disease transmission and infection rate are other influencing factors for tissue tropism. For example, although the influenza virus predominantly infects the upper respiratory tract, when it finds routes to transmit to the eye, the local infection can manifest into conjunctivitis.
Earlier research showed that the SARS CoV 2 invades the lung tissue through ACE2, causing inflammation in the respiratory tract. However, in the present studies, researchers show that SARS CoV 2 could have a broader tissue tropism and can infect cells other than through the ACE2 receptor. In other words, the viral protein may find matching patterns in other tissue cells as well.
They arrived at this conclusion by a detailed investigation of spike protein’s molecular structure. They used powerful scanning methods called X-ray crystallography and biochemical processes to view the protein structure’s atomic level arrangement. Their observations revealed that a tiny part of the spike protein structure — called cleavages — matched with the patterns on a receptor molecule called Neuropilin-1. Neuropilin-1 is found abundantly in the inner layers of blood vessels and tissue lining of many organs and helps form blood vessels and nerve connections.
The researchers detail that Neuropilin-1 has finger-like projections that are similar to an outstretched palm. On the spike protein, matching projections grab this hand and latch on to it.
From the collected data, the teams concurred that Neuropilin-1 could play a critical role in mediating viral entry access. They hypothesised that the coronavirus could be taking advantage of the Neuropilin-1 receptor molecule to sneak into host cells.
The nitty-gritty
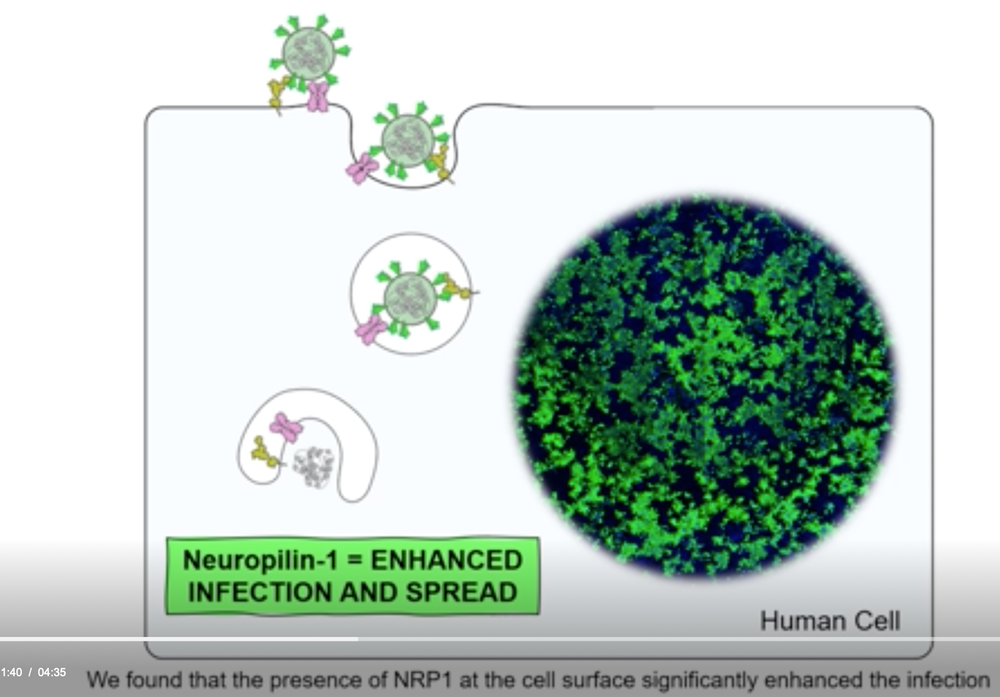
The teams conducted further experiments independently to check how critical Neuropilin’s role was in the infection cycle. One group from the UK investigated the degree of infection in human cells (lab-cultured cells) caused by the spike protein under three different conditions: only in the presence of ACE2, only Neuropilin-1, and both.
They found the spike protein present in cells with only Neuropilin-1, implying that the receptor facilitates viral entry. Also, the infection rate was highest when both the receptors are present in the cells, signifying the virus takes advantage of both pathways.
However, the degree of infection was lower with either of the receptors as compared to the presence of both.
Another group traced the spike protein’s path in the body of mice. They found it entered blood vessels and the neurons in the brain. When they examined the nasal tissues of Covid -19 patients, they were surprised to find that those cells of nasal tissue and brain that did not have ACE 2 but had Neuropilin -1 were positive for the spike protein. The spike protein was exhibiting broader tissue tropism.
Another team conducted a few more experiments to find a countermeasure to see if specific molecules mimicking antibodies could disrupt the binding of the spike protein and Neuropilin-1. They found that a molecule labelled EG00229 blocked the spike protein’s access to Neuropilin-1; the virus could infect fewer cells, thereby reducing the infection rate.
With these detailed results in hand, the authors conclude that Neuropilin-1 plays a crucial role in facilitating an alternate gateway for the SARS-CoV-2 virus.
It remains to be seen how emerging research will take advantage of these inputs to speed the design of effective therapies for Covid-19.
