
- Home
- India
- World
- Premium
- THE FEDERAL SPECIAL
- Analysis
- States
- Perspective
- Videos
- Sports
- Education
- Entertainment
- Elections
- Features
- Health
- Business
- Series
- In memoriam: Sheikh Mujibur Rahman
- Bishnoi's Men
- NEET TANGLE
- Economy Series
- Earth Day
- Kashmir’s Frozen Turbulence
- India@75
- The legend of Ramjanmabhoomi
- Liberalisation@30
- How to tame a dragon
- Celebrating biodiversity
- Farm Matters
- 50 days of solitude
- Bringing Migrants Home
- Budget 2020
- Jharkhand Votes
- The Federal Investigates
- The Federal Impact
- Vanishing Sand
- Gandhi @ 150
- Andhra Today
- Field report
- Operation Gulmarg
- Pandemic @1 Mn in India
- The Federal Year-End
- The Zero Year
- Science
- Brand studio
- Newsletter
- Elections 2024
- Events
Why women in Kerala are risking their lives with dangerous home births

In February of this year, tragedy struck when a 39-year-old mother and her newborn lost their lives during a poorly executed home delivery in Thiruvananthapuram. Despite the safer option of hospital delivery, the husband chose the riskier route, resulting in Shameera Beevi’s death due to excessive bleeding.Shameera’s husband Nayas now faces charges of culpable homicide. Her pregnancy...
In February of this year, tragedy struck when a 39-year-old mother and her newborn lost their lives during a poorly executed home delivery in Thiruvananthapuram. Despite the safer option of hospital delivery, the husband chose the riskier route, resulting in Shameera Beevi’s death due to excessive bleeding.
Shameera’s husband Nayas now faces charges of culpable homicide. Her pregnancy was deemed high-risk due to it being her fourth following three C-sections, with the most recent one just a year prior. Despite this, Nayas chose to proceed with a home delivery against the recommendations of ASHA workers, neighbours, and the ward councillor. The delivery was performed by Nayas' first wife, who practices acupuncture.
The incident ignited a contentious debate surrounding the legitimacy and medical safety of home birthing, questioning its efficacy in comparison to the modern healthcare provided by allopathy. According to healthcare workers who practice allopathy, the inclination towards riskier home births is gaining momentum, propelled by the dissemination of misleading information via social media regarding the advantages of 'natural' childbirth and the promotion of fear surrounding C-sections.
The 'comfort' of homes
Certain establishments are enabling such deliveries by providing access to traditional midwives and practitioners of naturopathy and acupuncture, despite cautionary advice from healthcare professionals. Nevertheless, the adverse outcomes for both mother and children frequently remain undisclosed until a calamitous event transpires.
Kerala is a state that takes great pride in achieving nearly 100% institutional deliveries. Since 2005, the proportion of institutional deliveries in the state has consistently been above 99.5%. According to the National Family Health Survey, 2015-16 and NFHS-5 2019-20, it had reached 99.8%. However, as per the annual state vital statistics report of 2021, the share of institutional (government and private hospital) births to total registered births dropped slightly to 98.81%.
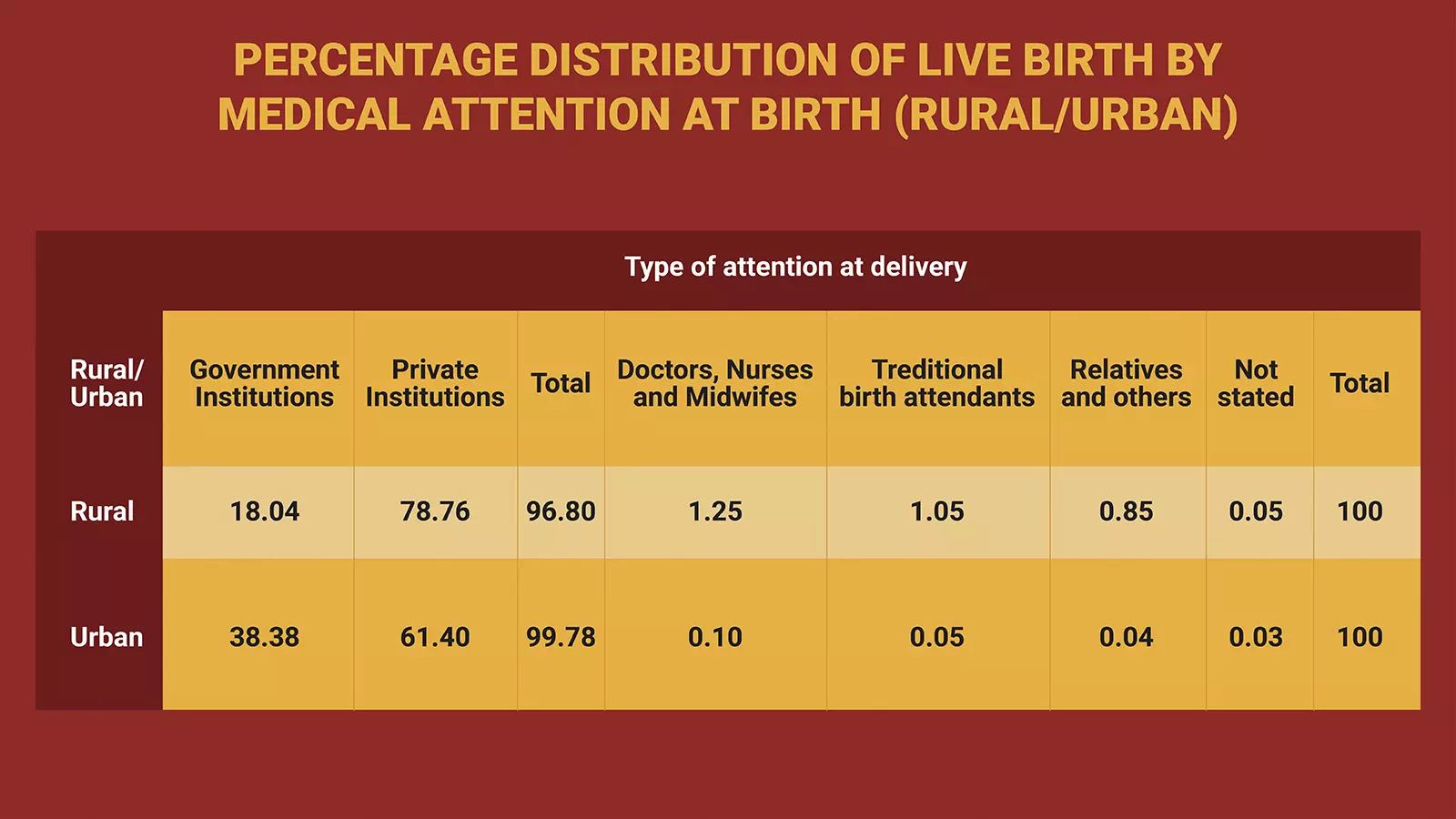
“Most of the deliveries in both the rural and urban areas are institutional deliveries. As many as 96.80% deliveries in rural areas and 99.78% deliveries of all the deliveries in urban areas were reported as institutional birth during 2021,” read the vital statistics report published in May 2023.
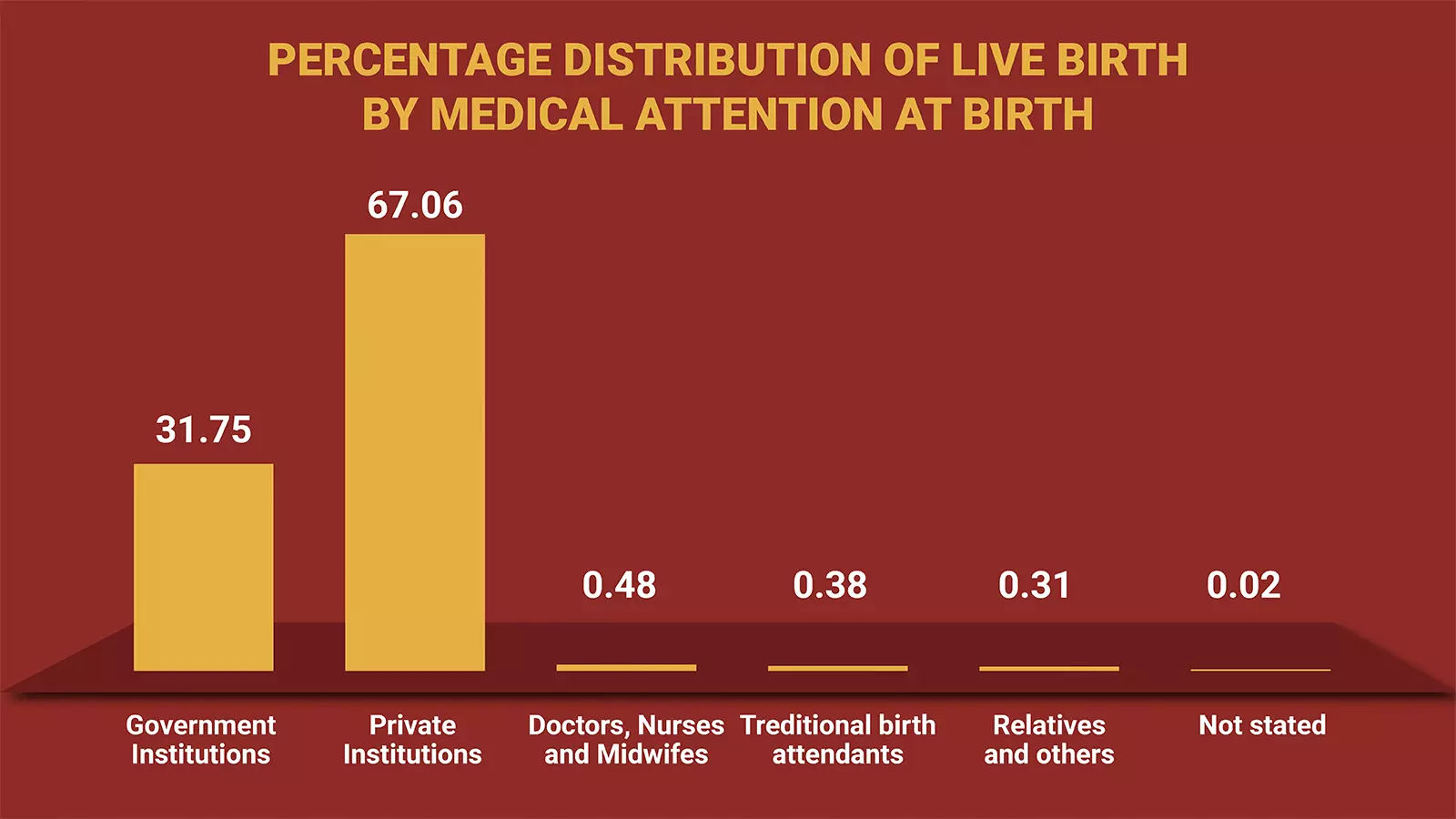
According to government records, 31.75% of live births are attended to in government hospitals, while 67.06% of mothers opt for private hospitals. The remaining deliveries that happen outside the healthcare system are distributed among various categories: 0.48% receive assistance from qualified professionals, 0.69% are assisted by untrained personnel, and 0.02% have not been specified.
While these figures might seem negligible from a national perspective, they raise concerns in a state that prides itself on its European-level healthcare standards.
“It is seen that out of 1,36,759 live births in rural area, 96.8% events are reported as institutional births and in the case of urban areas, the corresponding rate is 99.78%. In spite of having enough medical facilities across the state, a small percentage of live births (1.05%) is still attended by traditional birth attendant/relatives in rural area and 0.05% in urban area,” reads the vital statistics report for the year 2021.
During 2021, the percentage share of institutional deliveries to total live birth is 98.81%.
When one looks at the institutional births, it is seen that out of the 1,33,288 live births occurred in government hospitals, 55.87% are normal deliveries and 42.56% are caesareans. But in the case of private hospitals, out of 2,81,475 live births, the percentage of normal deliveries and caesareans is 52.87% and 43.29% respectively. It is also noted that in both types of births, the percentage of normal deliveries is more than that of caesarean.
These tiny fractions of deliveries, amounting to less than 1,000 annually, remain unnoticed by the state’s health system and occur outside healthcare facilities. Some of these cases involve “precipitous labour”, which is rapid and brief, often leading to sudden or inevitable home births due to swift cervical dilation and descent of the foetus into the birth canal.
Additionally, births that occur while en route to hospitals are categorised as home births by the health system. In certain tribal areas, home births are regarded as a cultural tradition. What worries the medical community is the trend of glorifying home birthing as a natural event and campaigns discouraging seeking medical assistance during pregnancy, including rejecting foetal imaging.
Kerala also boasts of a low maternal mortality ratio, recorded as 19 in the latest Sample Registration System (SRS) data. This achievement is attributed to ongoing efforts to develop safe delivery care services and implement quality improvement standards in obstetric practices throughout the state, aimed at identifying and addressing all potential causes of maternal mortality.
“It’s unfortunate that the glorification of home birthing persists in a state like Kerala, known for its advancements in education and healthcare. This happens because some folks promote ideas against modern medicine. Certain media also make it sound good,” opines Dr Jinesh PS a Melbourne-based surgeon from Kerala.
“This is not an isolated case; the endorsement of home birthing is observed in various sections, only garnering attention when mortality incidents arise. However, there is a glimmer of hope as the support for home birthing seems to be dwindling compared to a decade ago. It's widely recognised that home birthing increases the risks of maternal and infant mortality. Yet, there’s another aspect that is often overlooked. Hospital births facilitate the early detection and effective treatment of congenital diseases through newborn screening, crucial for infant health,” adds Dr Jinesh.
How women are pushed away
Even when doctors like Jinesh explain things logically, the fact that some people are still pushed away from the medical system because of undesirable attitudes from doctors and hospitals remains a sad reality.
Sija Sivadas, 41, a former Malayalam television journalist, chose to have all three of her babies outside of a hospital due to a negative experience with her gynaecologist during her first pregnancy in 2013. She gave birth to her first and third children at Birth Village in Kochi, a facility advocating and supporting assisted natural childbirth. Her second child was born at home, where her husband, a state government employee, aided her during labour.
“I suffered from severe Hyperemesis gravidarum, but instead of informing me about the condition and providing comfort, my doctor frightened me, pushing me into depression to the point where I contemplated terminating the pregnancy. I was even given Susten injections, typically reserved for women with a history of miscarriage, despite being a first-time mother,” Sija told The Federal.
She points out that there's a lot of wrong information prevailing about how pregnant women should act, stressing the lack of reliable knowledge.
“Each woman will experience signs of impending childbirth. However, hospitals often do not empower or encourage women to recognise these signs on their own. Rather, it is left to the discretion of doctors. Unfortunately, many doctors fail to acknowledge the uniqueness of each pregnant woman, treating them as standardised products from an assembly line,” she said.
“Our hospital system lacks a supportive environment for pregnant women. They neglect promoting trust in women’s instincts about their own bodies, instead prioritising compliance with doctors' directives.”
“The recent cases of maternal and infant mortality share some common traits. First, these mothers had limited education and relied on information from WhatsApp or YouTube. Second, they were not first-time mothers and had previously undergone C-sections. Besides, they did not follow proper diets or exercise routines. Lack of sufficient spacing between pregnancies also increased the risk of bleeding, particularly when babies were overweight and labour occurred soon after a C-section. I don't advocate for everyone to choose home birthing, but for those who prefer it, they should be well-educated about the process and their own bodies. Moreover, they should have strong support from their partners and be in a comfortable and supportive environment,” Sija suggested.
Why the risk
Health department data indicates a notably higher occurrence of home births in Malappuram compared to other districts, leading to an elevated risk of neonatal and infant mortality. Despite the safer alternative of institutional deliveries, numerous families in the district are choosing home births. This decision is influenced by several factors such as the undue influence of home birth practitioners and misunderstandings about childbirth. From 2021-23, there were around 536 home deliveries recorded in the district.
Dangerous examples
A recent Facebook post by an acupuncturist from Valancherry, Malappuram district, describing her experience of going into labour at home and delivering the baby “just like a soap bar slipping out of a hand”, went viral and received significant criticism. In her social media post, Hira Hareera asserted that she hadn't sought medical advice throughout her entire pregnancy. Despite experiencing a breach presentation, she didn't require any vaginal stitches and was able to walk within an hour after delivery. She shared a family photo with the newborn, indicating the birth time and the time of the snapshot with a gap of 1 hour 38 minutes.
Critics of Hira's promotion of childbirth without medical oversight argue that this trend may encourage more individuals to opt out of the healthcare system, potentially jeopardising Kerala’s lower rates of maternal and infant mortality.

The photo Hira Hareera posted after giving birth to her child at home.
In January 2018, a 23-year-old woman from Malappuram, Kerala, passed away following the birth of her first child at a naturopathy clinic. The clinic's protocol included the mother delivering her baby while standing in a tub of water. This was not the first case of maternal and infant mortality during attempted water birthing in Kerala.
“Engaging in such risky endeavours under the guise of naturopathy or any other pretext is completely devoid of scientific knowledge,” says Info Clinic, a voluntary online platform run by young doctors, providing regular insights on health and medical issues through social media channels. The utmost and maximum care should be provided to both the mother and the child during labour. Their lives should not be treated as experimental specimens. Administrators must not turn a blind eye to institutions operating without proper licensing or basic infrastructure in place,” says the doctor’s collective.
The Federal tried to contact health minister Veena George several times in this matter but she had not responded till the filing of the copy.
However, in a distinct initiative, the birth companion scheme, which was trailed at SAT Hospital in Thiruvananthapuram, which is the mother and children wing of Government Medical College Hospital, has proven to be immensely successful, as per the Kerala Health Department.
The initiative was to permit a close family member or female friend to accompany a pregnant woman into the labour room and stay with her through the entire birthing process. Although initially implemented as an experiment, it has been warmly received by female patients and their families, says a department of health press note.
