
- Home
- India
- World
- Premium
- THE FEDERAL SPECIAL
- Analysis
- States
- Perspective
- Videos
- Sports
- Education
- Entertainment
- Elections
- Features
- Health
- Business
- Series
- In memoriam: Sheikh Mujibur Rahman
- Bishnoi's Men
- NEET TANGLE
- Economy Series
- Earth Day
- Kashmir’s Frozen Turbulence
- India@75
- The legend of Ramjanmabhoomi
- Liberalisation@30
- How to tame a dragon
- Celebrating biodiversity
- Farm Matters
- 50 days of solitude
- Bringing Migrants Home
- Budget 2020
- Jharkhand Votes
- The Federal Investigates
- The Federal Impact
- Vanishing Sand
- Gandhi @ 150
- Andhra Today
- Field report
- Operation Gulmarg
- Pandemic @1 Mn in India
- The Federal Year-End
- The Zero Year
- Science
- Brand studio
- Newsletter
- Elections 2024
- Events
- Home
- IndiaIndia
- World
- Analysis
- StatesStates
- PerspectivePerspective
- VideosVideos
- Sports
- Education
- Entertainment
- ElectionsElections
- Features
- Health
- BusinessBusiness
- Premium
- Loading...
Premium - Events

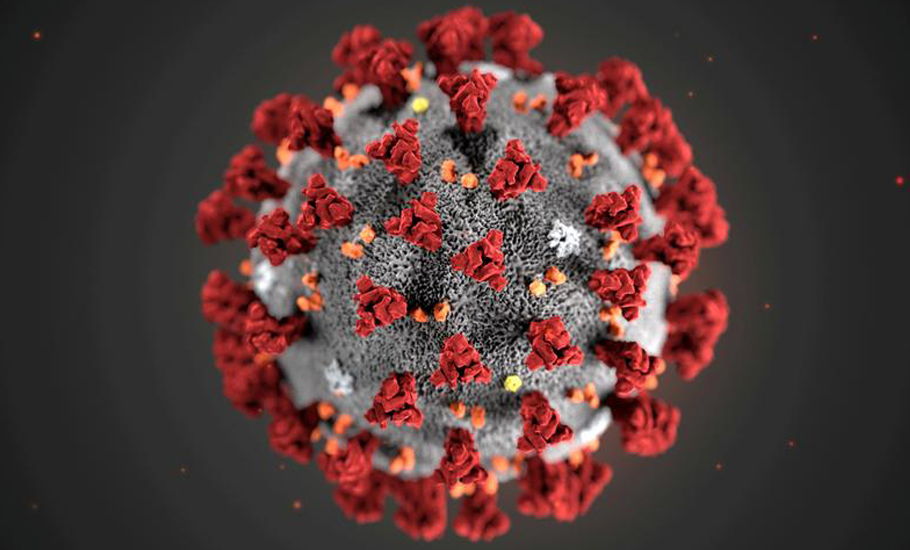
How a puff instead of a jab can fight Covid better

Despite initial enthusiasm that vaccines would wipe out the novel coronavirus and make it history has been humbled by the emergence of variants with immune escape mutations. Vaccines, available evidence shows, prevent severe illness, hospitalisation, and death. Still, almost all the Covid vaccines fail to arrest the infection and transmit emerging variants. Jabbing the vaccines in the...
Despite initial enthusiasm that vaccines would wipe out the novel coronavirus and make it history has been humbled by the emergence of variants with immune escape mutations. Vaccines, available evidence shows, prevent severe illness, hospitalisation, and death. Still, almost all the Covid vaccines fail to arrest the infection and transmit emerging variants.
Jabbing the vaccines in the muscle produces a cocktail of antibodies that seek and destroy the virus in the bloodstream. However, few of these antibodies reach the nose’s mucus, where the virus first gets its foothold. Alarmed at the rate of breakthrough infection caused by the Omicron variant, immunologists are looking towards an alternative route for immunisation—nose. They hope that the nasal vaccines provide the desired ‘sterilising immunity’.
Omicron
First detected in the specimens collected on November 11, 2021, in Botswana, the Omicron variant soon found its way across the globe, triggering the next wave of infections.
What made the Omicron break all barriers?
Prior infection, complete vaccination, hybrid immunity obtained from the combination of disease and vaccination, none could save one from the clutches of the Omicron. Seventy-two mutations throughout its genome, of which 30 amino acid substitutions, three small deletions, and a small insertion in the genome coding for spike protein, a critical surface protein that enables the virus to latch on and infect cells, indeed was an advantage for the variant. Crucially, the 15 amino acid substitutions in the receptor-binding domain (RBD), a region on the virus’s surface that facilitates its entry into the human cells, helped it dodge the antibodies from prior infection and vaccination. Assisted by the genome changes, the variant was more trenchant at reproducing in the upper airways, including the nose, throat, and mouth.
Nonetheless, it was less effective. Researchers found that the growth of omicron was 70 times more than other variants in the human airways tissue samples but was ten times less in the lungs. Relentless in multiplying in the upper respiratory tract, Omicron was about 4.2 times more transmissible and could infect six times as many people as Delta, resulting in a tsunami of Covid cases. With the rapid growth of the virus in the upper airways, but sluggish advancement in the lungs, often the infected experienced Omicron like a common cold with little or no damage to the lungs. Prior vaccination also helped. However, in rare cases, some needed to be hospitalised, and a for few, it was fatal.
Between the cup and the lip
A study led by Guruprasad Medigeshi, Translational Health Science and Technology Institute, Faridabad, Haryana, clearly showed the “Omicron variant of SARS-CoV-2 is capable of escaping immunity provided by currently available vaccines and even natural infection due to significant mutations in its spike protein.” An individual contracting infection after vaccination is called a ‘breakthrough infection’.
When infected or vaccinated, copiously produced neutralising antibodies clear the body of the virus. The strength of antibodies starts to wane with time yet linger in small quantities for many months. The immune system responds by producing more antibodies when infected again, trained and primed by prior natural infection or vaccination. However, it takes some time for antibodies to reach the threshold level. The time gap between the infection and the antibodies swelling to the threshold level decides if the breakthrough infection will be a typical or rare oddity.
Brisk growth of Omicron in the upper airways such as nose before the immune response could muster strength enabled it to sneak past the weak immunity from both vaccination and natural infection. While vaccines plunge into action before the infection spreads to the lungs, thus preventing severe illness and fatality, the nose and upper respiratory area, including the nose, tonsils and adenoids, remained susceptible as the initial point of infection. This resulted in breakthrough infection more commonplace with Omicron variant.
Enemy at the gate
Trained by vaccines, B Cells, a type of immune cells, churns out antibodies, mainly IgG, a potent weapon against pathogens. These antibodies, in small quantities, roam around the body through the blood in search of invaders. If the virus is detected, an alarm is raised, and the immune system is awakened. Another type of immune cell called T Cells help B Cells to produce antibodies in large quantities.

Further, the T Cells also assemble killer T Cells that search, seek and destroy the infected cells. The current vaccines, administered through intramuscular injection, are good in triggering the B Cell and T Cell response. Nevertheless, there is another poorly explored type of immune response, which the current Covid vaccines are unable to awake, arouse harness against the pathogen.
Open to the external environment, the nose, mouth, lungs, and digestive tract are constantly under attack by millions of microbes every second. A wet, mushy tissue lining the nose, mouth, lungs and digestive tract, warding off dirt and pathogens. The B Cells that hang around the mucosal tissues secrete a distinct antibody called IgA. The IgG secreted by the B Cells circulates in the blood and works like internal police to look for pathogens. Acting as a guard outside the gate, this IgA operates like border police, preventing the virus from entering the body. There are also specific types of T Cells, called tissue-resident memory (TRM) cells, that patrol the barrier sites such as the skin, genital tract and mucus linings.
Nose, the trojan horse
Long-lasting immunity for many respiratory infections from vaccination and natural infection is hopeless. Coronaviruses replicate in the upper and lower respiratory tract, making it more difficult. Vaccine-induced or after natural infection, there is an appreciable level of antibody circulation in the lungs. However, on the surfaces of our nostrils, the levels of antibodies are scanty. Thus, the vaccine effectively blocks severe disease of the lungs because there are appreciable levels of antibodies in the lower respiratory tract. Devoid of antibodies, the nose and the upper airways remain vulnerable. Chasing ‘sterilising immunity’, researchers focus on deepening the immunity in the moist surfaces of the mucosal linings of the nasal airways.
When the vaccine is administered, the immune response shapes the antibody to fit the antigen of the specific pathogen. Neutralising antibodies such as IgG and T Cells particular to the pathogen evolves. When the vaccine is administered in arms, the mucosal immune cells are not exposed to the antigen. Hence the IgA antibody and tissue-resident memory T Cells are underdeveloped. On the other hand, the intranasal vaccine can stimulate neutralising IgG, mucosal IgA, T Cell responses and tissue-resident memory cells, essentially blocking both the infection and transmission, providing ‘sterilising immunity’.
Shot in the arm
A little more than142 vaccines are being developed worldwide to fight against Covid. Eleven were abandoned after trials for failing to elicit requisite immunity. Of these, 16 are authorised or approved worldwide. An additional 115 are under various stages of clinical trials after proving to be viable in animal and laboratory studies.
In January this year, the Indian drug controller gave full approval to ICMR-Bharat Biotech’s Covaxin, the University of Oxford, and AstraZeneca’s Covishield. The Sputnik V (also known as Gam-Covid-Vac) DNA based Ad26 and Ad5 adenovirus vector vaccine was the third one to get authorisation. Zydus Cadila’s DNA-based vaccine delivered by a skin patch ZyCoV-D, developed with the assistance of the Department of Biotechnology, Baylor-Biological E’s protein-based vaccine Corbevax and Novavax-Serum Institute’s Covovax were recently given emergency use approval in India. Moderna’s spikevax, Johnson and Johnson’s vaccine, Pfizer-BioNTech COVID-19 Vaccine are also formally approved in India but hardly available.
At the time of writing, about 174 crore vaccine jabs have been administered, whooping 84 per cent is Covishield and 15.65 per cent Covaxin. Sputnik V is just 0.3 per cent, and the other vaccines put together account for less than 0.05 per cent.

All these vaccines are more or less administered through intramuscular injection. Vaccines given at the arm muscle, called the deltoid, travel to the clusters of lymph nodes are located under the armpit and trigger immune response and create immunological memory. Nonetheless, the vaccines administered through muscle have a vital shortcoming against respiratory pathogens; they can still enter the mucosal lining in the respiratory tract, causing infection. This was evident from the Omicron induced pandemic tsunami.
Why prick, if puff is better
Intranasal vaccines have a considerable advantage over the vaccines that need to be injected into the arm. They do not need syringes, hence less cost and lesser medical waste to manage. They can be easily administered to children and those with a phobia of needles. One does not require trained paramedical staff to help a few drops of vaccines inside the nasal cavity. Thus poor and underdeveloped countries could use trained health volunteers to deliver the vaccine.
Nevertheless, developing an intranasal vaccine is ardours. The research on intranasal vaccines using inactivated viruses has been disappointing. Only modified live virus vaccines have shown modest results. We are not clear if the mRNA, DNA, protein type vaccines could penetrate the mucociliary blanket covering the upper airways to trigger the immune response. The vaccines must deliver an adequate amount of antigen to penetrate the mucus barrier to start a desirable level of the immune response. This is not the case with vaccines delivered through the muscle. By analysing the blood samples, the levels of IgG antibodies can be measured. However, measuring mucosal antibodies is demanding. The amounts of IgA are low, fluctuating and hence difficult to quantify. A waft of tasty food smell could flood the mouth with saliva, diluting the levels of the antibodies.
Until now, only one vaccine, FluMist, made from the weakened flu virus, uses the nasal path. Nonetheless, the vaccine works wonders in unexposed children, but its efficacy is dismal among adults. Yet several efforts are on to develop a viable nasal Covid vaccine. Bharat Biotech’s BBV154, aka ChAd-SARS-CoV-2-S, seems promising. The nasal vaccine cleared the virus in mice, hamsters, and macaques in the lower and upper airways.
Developed with the support of the department of biotechnology (DBT) and Biotechnology Industry Research Assistance Council (BIRAC), the vaccine is in the clinical trial phase II. The UK, Codagenix’s nasal vaccine, COVI-VAC, partnered with the Serum Institute of India, is currently in phase I clinical trial.

Beijing Wantai Biological Pharmacy Enterprise, Xiamen University, and Hong Kong University spray vaccine use a live-attenuated influenza virus modified to express spike protein of SARS-CoV-2 is under clinical trial phase I. In addition, a few more nasal vaccines are under development in the US, Cuba, and Iran
Most of these nasal vaccines have been very effective in animal studies. However, what works for animals may not pan out to humans in vaccine development. Questions and hope still remain; will they work by providing sterilising immunity, along with preventing death and severe illness, for a suitably long time? Will they work against emerging variants? Will they have a space as already massive doses have been administered?
