
- Home
- News
- Analysis
- States
- Perspective
- Videos
- Education
- Entertainment
- Elections
- World Cup 2023
- Features
- Health
- Business
- Series
- Economy Series
- Earth Day
- Kashmir’s Frozen Turbulence
- India@75
- The legend of Ramjanmabhoomi
- Liberalisation@30
- How to tame a dragon
- Celebrating biodiversity
- Farm Matters
- 50 days of solitude
- Bringing Migrants Home
- Budget 2020
- Jharkhand Votes
- The Federal Investigates
- The Federal Impact
- Vanishing Sand
- Gandhi @ 150
- Andhra Today
- Field report
- Operation Gulmarg
- Pandemic @1 Mn in India
- The Federal Year-End
- The Zero Year
- Premium
- Science
- Brand studio
- Home
- NewsNews
- Analysis
- StatesStates
- PerspectivePerspective
- VideosVideos
- Entertainment
- ElectionsElections
- Sports
- Loading...
Sports - Features
- BusinessBusiness
- Premium
- Loading...
Premium
What simple mathematics can tell us about coronavirus

As on March 26, 2020, the novel coronavirus pandemic (COVID19) has killed 18,589, and infected 4,16,686. Every minute, the virus is claiming more lives. Before we are convinced of the savagery of the novel coronavirus pandemic, let us look in comparison, say, the deaths caused by road accidents. The epicentre of the novel coronavirus, China, has a mortality of 700 people per day. That would...
As on March 26, 2020, the novel coronavirus pandemic (COVID19) has killed 18,589, and infected 4,16,686. Every minute, the virus is claiming more lives.
Before we are convinced of the savagery of the novel coronavirus pandemic, let us look in comparison, say, the deaths caused by road accidents. The epicentre of the novel coronavirus, China, has a mortality of 700 people per day. That would be 2,55,500 deaths in a year. The actual total deaths in China caused due to the novel coronavirus, 3,277, pales before this figure. And around 50,000 people die every year in India due to snakebites alone.
Given such a relatively low death rate due to coronavirus, why is there a worldwide panic?
Tantalizing conspiracy theories are brandished on social media: plot by Illuminati to cull the human race, deliberate strategy by China to topple the USA and emerge as a world political and economic power, nature’s vengeance on us for not living in harmony with mother Earth. These fairy tales are childish. Keep them aside.
Recent research published in estimate the Case Fatality Ratio (CFR), percentage of deaths from confirmed cases of the infection, of novel coronavirus as 1.4%. The CFR of SARS, MERS is much higher. Deadly viruses like Ebola can kill as much as 80% of the infected. Compared to them, the novel coronavirus is docile.
Why, despite the low mortality rate, are healthcare workers, and humanitarians worried? The answer lies in simple mathematics.
Public healthcare infrastructure
To understand the problem at hand, let’s look at Chennai, a South Indian metro with a population of one crore people. Government hospitals in Chennai have 12,522 beds and in private hospitals, 8411 beds. Let’s say 21,000 beds in total.
In 2018, the statistics say 1,260 people were killed, and 7,438 people were injured in a road accident. Due to these accidents in a year, 8,698 patients would have required medical treatment. That is about 24 people per day. Admitting 24 new patients tomorrow is not going to be an issue. There are adequate medical infrastructure and medical personnel to attend them.
Now imagine that all the road accidents that were supposed to take place over a year happened in one day. One fine morning, 8,698 people throng hospitals, both government and private. Surely, some might only require cursory wound dressing, some minor treatment, and a portion will need trauma care, including brain surgery.

Representational Photo: PTI
On any given day, how many of the 21,000 beds will be empty? How many ICU beds would be at the disposal? Will there be enough surgeons to attend to trauma? From wound dressing, bone fracture plaster casts to simple sterilized medical equipment shortage would ensue. The medical establishment would be overwhelmed, and a lot more will die due to lack of proper medical care. Avoidable deaths would occur.
The same number of accidents if spread over a year, can be well managed. Even if a major disaster occurs and injured are ten times the daily rate, the hospital facility can be stretched to meet the abrupt demand.
Road accidents do not spread to others; snakebites are not contagious. However, infectious diseases like COVID-19 spread, and transmit in a population like wildfire. Transferred from one person to another, germs infect more and more people in the process.
How does this transmission take place?
Every infectious virus has two intrinsic properties — R0 (pronounced R nought) which is the basic reproduction number, and the Case Fatality Ratio, fraction of the infected host mortality.
The R0 value can be looked at as the intensity of the infectious disease outbreak. Higher the R0 value of a disease, the faster the disease would spread among the population. In simple terms, the value of R0 is equal to the number of newly infected cases, on average, an infected person will cause.
The R0 for measles ranges from 12–18, depending on factors like population density and life expectancy. This shows measles that is a highly infectious disease. If one person gets it, then about 18 will follow. Compared to measles, the novel coronavirus virus is less contagious. As this virus is new, we are not conclusive, but from the evidence we have, the R0 ranges from 2.2–2.6.
Several factors come into play in determining the R0. The incubation period, host density, modes of transmission — all affect the R0. Studies show that the novel coronavirus can travel only about a meter in air as compared to 100 meters range for airborne disease like measles. Second, the measles-causing germs can live outside the host for hours. In contrast, the novel coronavirus can survive only for 3 hours in air.
The public health advisory, that if you are compelled to step out of your house, say to purchase essentials like milk or grocery, maintain a distance of one meter, to avoid the spread of novel coronavirus, now makes sense, doesn’t it?

This R0 value, however, is only an average estimate. For some still mysterious reason, some infected persons, called super-spreaders, can infect a lot more. A woman in South Korea, who belonged to a religious sect, affected 37 people during church services (ironically, the service was held to obtain god’s grace to protect them from coronavirus). Which is why public gatherings are forbidden; we do not want to even accidentally trigger the hidden super-spreaders.
Case fatality rate (CFR)
Not every person who encounters an infectious germ dies. If all infected host die, then the virus cannot survive. From this point of view of evolution, that is not a desirable state for the virus. Hardly a deranged virus goes berserk and wipes out all the hosts it infects. Mostly the virus evolves to develop into a strain that can maintain a balance with the host. After all, the replication and survival is the name of the game in evolution for all organisms.
The case fatality rate or CFR is a fraction of the total deaths caused by the infection by the total number of hosts infected. This varies from one virus to another.
Also, the CFR or a particular viral disease is not ironclad. This number depends on a lot of factors such as the quality of medical and healthcare systems. Better availability of quality and affordable health care system in a particular region can reduce the CFR of a specific viral disease. Vaccination, development of more potent medicine — all contribute to mitigating the CFR.
In general, in the recent past, due to the advancements of science and technology, more people die at war than due to diseases. This was not the case before WWII. Universal and free healthcare do wonders in further improving public health.
A bit of mathematics
Given below is a list of some germs with their R0 and CFR values (note: these numbers are indicative and are subject to change based on the geographical location):
How fast does COVID-19 spread?
We saw that the R0 value of the novel coronavirus is around 2.6. If we do not control the spread of the disease, then one infected person would transmit to 2.6 other people (1 x 2.6). These 2.6 people will then again spread to 2.6 more people. So now in the third transmission level, we will have 1 x 2.6 x 2.6 = 6.76 infected persons. In the next spread level, 17.576 people would be affected. Not a big deal. We will remain smug. The fourth, fifth, sixth transmission, we would not even pay attention. The numbers are so low. Who cares if three hundred are infected in a country of 1.38 billion people?
But then the numbers seem to go crazy. Our stomachs start churning.
Look at this table. From one to 12th spread, how the numbers grow.
1
2.6
6.76
17.576
45.6976
118.81376
308.915776
803.1810176
2088.27064576
5429.503678976
14116.7095653376
36703.44486987776
95428.956661682176
By the tenth transmission level, the numbers are beginning to get worrying, right? The infection will snowball and ravage. In the 12th transmission, around 95,428, that is about one lakh people will be affected!
By then, the time is lost. Game over.
Notice the way the number rises; this is known as exponential growth.
Why worry?
After all, 80% of those infected need hardly any medical care. Just 20% need medical advice and about 5% hospitalisation. The CFR of novel carnivorous is only 1.4%. Even if a lakh is infected, what is the catch?
The above table is the number of infected new cases in that round. However, the total of infected persons is cumulative. That is, after the second spread, we have 2.6 from the first spread, and 2.6+2.6 from the second spread, total 9.36. In the third spread 2.6 + 6.76 + 17.576 = 26.936.
By the 12th transmission, the total number of infected people will be 1,55,070. This is around one per cent of Chennai’s population! Out of this, 20% would require hospitalisation (the rest 80% would only have a minor cold or so). Twenty per cent of 1,55,070 is 31,014. But remember, we only have 21,000 beds in Chennai! Of these 31,014 people, 7,288 (5%) would require severe intensive treatments. All these numbers are solely based on just 12 transmission cycles. Imagine what would happen if we let this cycle continue on without any control!
The affliction caused by the virus is just a cluster of severe respiratory illness. This could aggravate into dyspnea, difficulty in breathing and pneumonia. The critical stage could develop into acute respiratory distress syndrome. Most of these are treatable, provided we have adequate ventilators, ECMO machines and trained medical professionals.
Therefore, the actual problem with this pandemic is not the difficulty of medical care, but the exponentially increasing number of new cases each day that would cry for medical help.
Under the burgeoning burden, the healthcare infrastructure of even rich developed countries like Italy is crumbling. Shortage of medical equipment and staff, despite doctors and nurses working on it day and night, is found to be inadequate to meet the demands. They had abandon treating those who are eighty and above.
China had to build two hospitals with thousands of beds each, well stocked with ventilators and ECMO, especially to treat COVID-19 patients, in just ten days. Makeshift medical treatment centers for those who did not show acute symptoms were made in 17 sports stadiums, each having a capacity to provide treatment to 1,000 people. Medical professionals and staffs were sourced from other regions to Wuhan, the epicentre of the pandemic. The tide of new patients arriving at the hospital doors was managed.
Whataboutery
Seasonal flu is also a viral infectious disease transmitted from person to person. It occurs every year. But why do we hardly miss sleep over it? The secret is hidden in its R0 value. The R0 of seasonal flu is 1.3. It is half that of novel carnivorous. One infected person will on to transmit it to 1.3 people and so on, on an average. Can you guess what would be the cumulative total number of an infected person after 12th transmission?
Hold your breath! It is 96.6250. Yes, you did read it correctly, just ninety-six people. This is why we scarcely bother and hardly pay attention. It is not a substantial public health challenge.
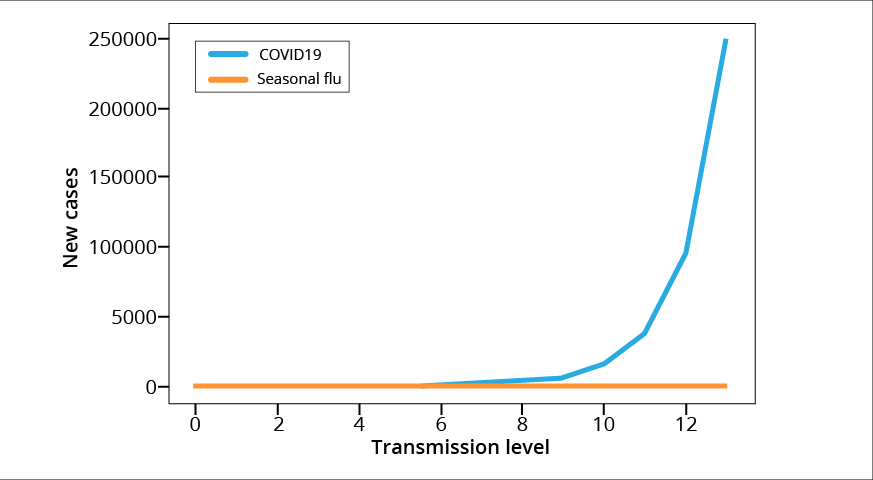
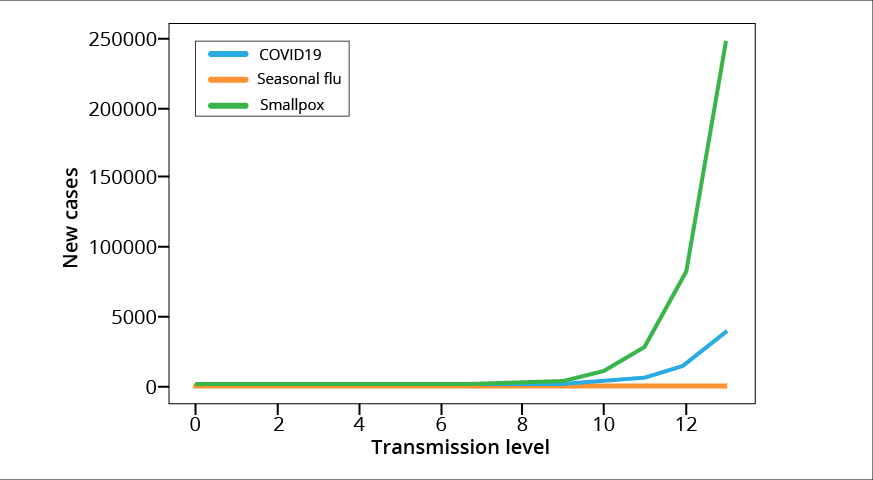
The graphs below show the exponential rise of newly infected cases at every transmission level due to COVID-19 as compared to seasonal flu. Look at how the increase in number of infected people is negligible for seasonal flu. In the scale of COVID-19, it is absolutely nothing!
Break the chain to stop the high transmission rate!
Viruses need a host to survive. The virus can survive in an infected person only for the incubation period. For novel coronavirus, it is about 14 days. Thus, this virus (just like every other virus) will need new hosts to survive.
If an infected person is identified early and placed in quarantine, s/he cannot spread. There is a catch. Not all infected persons show typical symptoms. Further, most of the symptoms are very similar to seasonal flu that we need an additional test to confirm coronavirus infection.
To add to the frustration, recent evidence suggests that some people infected with the virus are asymptomatic but can still be contagious. This is why physical distancing is advised. A person whom we meet may show no symptoms yet could be a carrier happily spreading the virus. Keeping safe distance and washing hands thoroughly with soap for 20 seconds and covering our mouths and nose when coughing and sneezing will help slow the pace of the spread of the germ and break the chain.
If the situation warrants, as in India today, extreme steps like lockdown of a whole region would become imperative. By these measures, we are slowing the spread and thus reduce the number of new patients who seek medical help, providing a breathing space to the medical infrastructure to cope up.
Besides, when the virus spreads fast, it may also mutate into new lineages. Some researchers claim the devastating effect of the illness we see in Italy may be due to a deadly mutation while spreading. Hindering the spread perhaps may also arrest the emergence of more virulent lineages.
Physical distancing but social solidarity: Call of the time
Participation of every single individual is a must to break the chain and stop the spread of the virus. Not everyone can afford the luxury of work from home. Poor people who eke out a living on daily wages will find it harder. Construction workers, vegetable sellers, flower vendors and their like would find it difficult. Government and civil society must compensate them for the loss of work. But, stay at home, we must.
Just a hundred years ago, the Spanish flu, another contagious disease caused by a virus, killed about 1.7 crore people in India, about two in thirty people. They lacked our knowledge of the virus, its epidemiology. We now know a lot more on how the germ spreads and how we can arrest it. We must act based on this knowledge.
Battle against the deadly pandemic cannot be waged in hospitals alone. We must fight by remaining in our homes. It is only in our collective action we can redeem from the epidemic. The vulnerable are old, people with prior illness, and the poor. Lacking in nourishing food, poor in general have low immunity. We should behave compassionately and with consideration, especially in these trying times. For instance, by permitting paid leave to domestic workers, maids, buying from local fruit and vegetable vendors, local small scale businesses, and so no, we can do our bit.
(The author is an evolutionary biologist at Department for Evolutionary Theory, Research Group Theoretical models of Eco-evolutionary Dynamics, Max Planck Institute for Evolutionary Biology, Plön, Germany)

