
- Home
- News
- Analysis
- States
- Perspective
- Videos
- Education
- Entertainment
- Elections
- World Cup 2023
- Features
- Health
- Business
- Series
- Economy Series
- Earth Day
- Kashmir’s Frozen Turbulence
- India@75
- The legend of Ramjanmabhoomi
- Liberalisation@30
- How to tame a dragon
- Celebrating biodiversity
- Farm Matters
- 50 days of solitude
- Bringing Migrants Home
- Budget 2020
- Jharkhand Votes
- The Federal Investigates
- The Federal Impact
- Vanishing Sand
- Gandhi @ 150
- Andhra Today
- Field report
- Operation Gulmarg
- Pandemic @1 Mn in India
- The Federal Year-End
- The Zero Year
- Premium
- Science
- Brand studio
- Home
- NewsNews
- Analysis
- StatesStates
- PerspectivePerspective
- VideosVideos
- Entertainment
- ElectionsElections
- Sports
- Loading...
Sports - Features
- BusinessBusiness
- Premium
- Loading...
Premium

Are COVID-19 vaccines working? Here's what no one is telling you

On December 8, 2020, 91-year-old Margaret Keenan, a grandmother in the UK, received the first Covid-19 jab as part of a mass vaccination programme. Within 10 months, on September 10, 2021, about 233 crore people worldwide, or about 29.9% of the world’s population, were administered both doses of Covid-19 vaccine. Global studies clearly show that vaccination protects from hospitalisation...
On December 8, 2020, 91-year-old Margaret Keenan, a grandmother in the UK, received the first Covid-19 jab as part of a mass vaccination programme. Within 10 months, on September 10, 2021, about 233 crore people worldwide, or about 29.9% of the world’s population, were administered both doses of Covid-19 vaccine.
Global studies clearly show that vaccination protects from hospitalisation and death. However, several questions still remain. How long will the vaccines give protection? Do we need to take a booster dose? If one had a prior infection, is it necessary to take the vaccine? The emergence of immune-escape variants of concern has only exacerbated these concerns.
Neither the crystal ball nor the armchair speculations are going to be of any aid here. Only by collecting data painstakingly, regularly measuring the immune response and conducting human and animal trials can we arrive at a reasonable answer for our worries. Here is what we have learnt in the past few months from studies conducted across the world.
First, a piece of good news. Putting to rest earlier fears that the protection conferred by the vaccine will last only for a short duration, three recent studies have shown that the effect of the COVID vaccine would most likely last the lifetime. With one caveat. The vaccine in the circulation seems to be effective against most of the current variants. It provides at least some level of protection against all of them. However, this vaccine’s efficacy will last only as long as coronavirus does not evolve into a new strain.
Immunology 101
Before we proceed to take a peek at the results of the studies, a quick recap of how the immune system works. Two armies of immune cells, innate and acquired, help us fight trespassing infectious pathogens. When the body is assailed by bacteria, a virus or parasite, the immune alarm goes off, triggering a series of cellular immune activities. The innate immune cells, such as macrophages, basophils, dendritic cells or neutrophils, are the first to respond. These innate immune cells are like general-purpose local police deployed for routine law and order maintenance. These immune cells do the job, and the invader is usually prevented from infecting.
However, innate immune cells are flummoxed; when the pathogen comes disguised to resemble human cellular parts, and the attack is more sophisticated, it becomes tricky. The spike protein of the coronavirus has features called ‘receptor binding domain’ that can stick to the ACE2 receptor on the human cell surface. These sneaky germs slip through the security cordon. Only special squads, armed and trained to catch these stealthy pathogens, can track, trace and target them.
When the body needs a more robust immune response, it turns to its adaptive immune cells, T-cells and B-cells. There is a division of labour between T cells, which destroy infected cells from the inside, and B cells, which produce antibodies that clean up free-floating viruses outside the cells. These cells are like the special-ops group of security services.
If you get COVID after vaccine it will be:
Mild or
Asymptomatic
Less risk of hospitalizationThis is an analysis of >120,000 ppl with less than 1% breakthrough COVID
Anecdotal post-vaccinations cases don’t tell the full story https://t.co/wVgwNsHa4g
— Faheem Younus, MD (@FaheemYounus) September 8, 2021
B-cells produce Y-shaped proteins called antibodies, which are specific to each pathogen. The neutralising antibody, which has high affinity, locks on to an antigen on the surface of the invading pathogen. Once the antibody latches, then that pathogen is marked for destruction. Macrophages and other immune cells crowd these germs and destroy them.
There are two main types of T-cells: helper T-cells and killer T-cells. Helper T-cells recognise the antigen on the surface of the pathogens and stimulate the B-cells to make antibodies. Killer T-cells directly destroy the infected cells. They also release cytokines, messenger molecules that trigger the immune system to respond to the emergency. Meanwhile, the immune system makes memory B cells and memory T cells that retain the information to ward off future infection by that specific pathogen.
Vaccines work by mimicking the immune system. The inactivated whole virus, or the virus part, administered as a vaccine, fools the immune system into thinking that it is under attack by a harmful pathogen. The alarm is raised, and like a mock drill, all processes are initiated. Helper T cells take the antigen to B cells, which in turn develops neutralising antibodies. Subsequently, memory B cells and T cells are formed. When that pathogen tries to slip in, the immune system wastes no time to retaliate. B cells and T cells proliferate, neutralising antibodies are churned out, the germ hardly gets a foothold.
Is innate immunity sufficient?
Every moment of our life, we encounter potentially harmful pathogens, like viruses, bacteria or fungi. Yet, we do not fall sick, thanks to the working of the innate immunity. We keep the constant bombardment of germs at bay through secretions of mucous, bile, gastric acid, saliva, tears, and sweat, and complement it by a general immune response such as inflammation. However, germ-causing diseases sometimes dodge the innate system, like a furtive intruder carrying a fake identity card, to infect. For example, the V protein of paramyxoviruses mimics IRF3 human protein to gain entry and cause infection.
What about coronavirus? Is the innate immunity adequate to arrest the infection? Akiko Iwasaki, the Waldemar Von Zedtwitz Professor of Immunobiology at Yale, conducted experiments on mice to determine which immune responses played the most critical role in COVID-19 cases. In the mice with neither T cells nor B cells, the infection persisted, showing that innate immunity is wanting, and adaptive immunity is needed to control primary infection. T cells and B cells can be triggered only by actual infection or by vaccination. Eating garlic, drinking green tea, and gargling with warm water is no substitute. The so-called immunity boosters against COVID 19 are but a chimaera.
Take-home message: Without triggering T cell and B cell response, either by infection or through vaccination, one cannot be fortified from Covid-19.
How good is the immune response from infection
When infected, the immune system germinates pathogen-specific B cells, T cells and memory cells. While natural immunity from measles is pretty solid and lasts a lifetime, natural immunity against influenza is weak. Why it is so, we are yet to fathom. However, how strong and persistent is the natural immunity from Covid-19?
A study conducted by researchers at The Rockefeller University, New York, NY, USA, shows that recovered patients have appreciable levels of antibodies and immunological memory even after 12 months of infection. The study involved 87 individuals who had recovered from Covid-19. Blood samples were drawn from them after six months of recovery. However, only 63 came back for the 12-month visit. Out of this 63, 28 had taken at least one dose of the mRNA vaccine, and the remaining 35 had not. Hence the researchers could analyse the relative levels of antibodies in the unvaccinated and vaccinated post-infection.

The antibody reactivity, neutralising activity, and the number of RBD-specific memory B cells remained relatively stable even after 12 months in both the unvaccinated and vaccinated groups. However, the antibody reactivity, neutralising activity, and the number of RBD-specific memory B cells were much more robust in the vaccinated group. Compared with unvaccinated participants, those who had received at least one dose had higher levels of antibodies and a nearly 50-fold increase in neutralising activity.
In short, even a single dose of an mRNA vaccine in individuals with past COVID-19 infections seem to provide enhanced immunity. The study showed that this hybrid immunity, which is a combination of immunity to COVID-19 derived from a previous infection and vaccine-induced immunity, also offers protection against the emergent variants of concerns, which the natural immunity could not provide.
Take-home message: If you have had Covid-19, then it is better to take the vaccine to boost the neutralising activity. The hybrid immunity protects you, at least partially, against the emerging variants of concern.
How persistent is vaccine-induced immunity?
After vaccine rollout, usually vaccinated people are closely watched to see if any of them come up with the disease. Also, researchers monitor the antibody levels in a select sample. Such studies conducted across the globe clearly show that vaccines confer very high levels of protection against severe illness and mortality from Covid-19. Nevertheless, the strength and persistence of the immune response was an open question until an innovative study found essential clues. The crucial research looked at the formation and persistence of vital germinal cell centres in the lymph node.
A dog can be trained to sniff a snake in a farmer’s field, bark at a burglar, follow the scent trail to chase the culprit or detect explosives. Whatever be the task, the dog has to be trained for that particular job. Likewise, the B cells have to be prepared to specifically recognise coronavirus. The training of the B cells occurs in a temporary structure in the lymph nodes called germinal centres.
Hundreds of lymph nodes are found throughout the body, including the neck, armpit, chest, and abdomen. Substances travelling through the lymphatic fluid are filtered at the lymph nodes, and infectious germs are identified. If that germ was encountered previously, memory B cells and memory T cells are most likely available. The immune system jostles the information from the immune memory cells to produce neutralising antibodies and appropriate T cells.
When one of the 500-odd lymph nodes in our body detects an unknown disease-causing pathogen, appropriate germinal centres emerge. Based on the antigen on the pathogen’s surface, the germinal centres produce slightly varied forms of B cells. Each form is pitted against the antigen of the pathogen. Through a fierce selection process, the best immune cells are selected. ‘Trained’ or affinity-matured B cells evolve in this process. These B cells can produce neutralising antibodies that can latch on to the virus firmly. Further, our immune memories are formed in the germinal centres. The vaccine also triggers the emergence of germinal centres.
Researchers at Washington University School of Medicine in St. Louis enlisted 14 people who received the mRNA vaccine. They sampled minuscule germinal centres in lymph nodes in the armpit, three weeks after the first dose, before the second dose, and at four, five and seven weeks. Samples were collected from 10 people after 15 weeks. All these participants had no prior Covid-19 infection; therefore, any immune response is only due to mRNA vaccines.
With just the first dose, the germinal centres formed in all 14 participants. They were producing B cells and antibodies that target the critical proteins of coronavirus. After the booster second dose, the response was enhanced and stayed high. After 15 weeks of the first dose, the germinal centres were still highly active, and the memory cells that recognised the coronavirus had not declined.
Of course, the study did not compare the formation of germinal cells in unvaccinated but naturally infected persons. Such a study is complex. During infection, the germinal centres usually form in the lungs. Taking samples from lungs is not child’s play. Although these studies were carried out with mRNA vaccines, Covaxin, Covishield, and Sputnik V, they have not been subjected to such analyses. Nevertheless, from our knowledge of immunology, we can be reasonably confident that results are unlikely to be divergent.
The message is clear: vaccination induces long-lasting germinal centres. The more prolonged the germinal centres work, the stronger and more durable our immunity will be. B cells emerging out of these long-lasting germinal centres can recognise a diverse set of viral genetic sequences. This means, such an affinity- matured B cells have a greater chance to thwart variants of the virus that may emerge.
Take home message: The vaccine clearly adds benefit, even to those with prior infection, conferring at least partial protection against emergent variants.
When does the vaccination take effect?
One of the studies looked at the antibody levels in the blood samples of vaccinated individuals. In people without prior exposure to the virus, antibody levels rose slowly after the first dose. After one week of the second dose, the levels peaked. Among the previously infected, as expected, the antibodies were present even before the first dose. Their levels shot up quickly after the first dose and peaked higher than the uninfected participants’ levels.
Which is paramount: T cells or B cells?
Which is controlling primary infection, reinfection, and vaccine-mediated protection; T cells or B cells? To understand this, Akiko Iwasaki and her colleagues used mice to study the effect of lack of T cells and the absence of B cells on the infection and reinfection.
First, they asked if B cells are needed to restrain primary infection. When they tested mice devoid of B cells, the viral clearance was only slightly delayed. Thus B cells are not necessary for controlling primary coronavirus infection. That is, during the acute infection, both T cells and B cells are adequate.
What about long term immunity. In the reinfection, is it the T cells or the B cells that are vital? When they reinfected the mice lacking T cells with coronavirus, the antibodies, even without T cells, could provide adequate protection. Highly immune evasive variants were also controlled by robust antibodies. In short, while T cells play a role during acute infections, our antibodies are crucial for long-term protection against reinfection.
Take home message: All vaccines are known to elicit good B cell response and hence, are most likely to confer protection against severe disease and death.
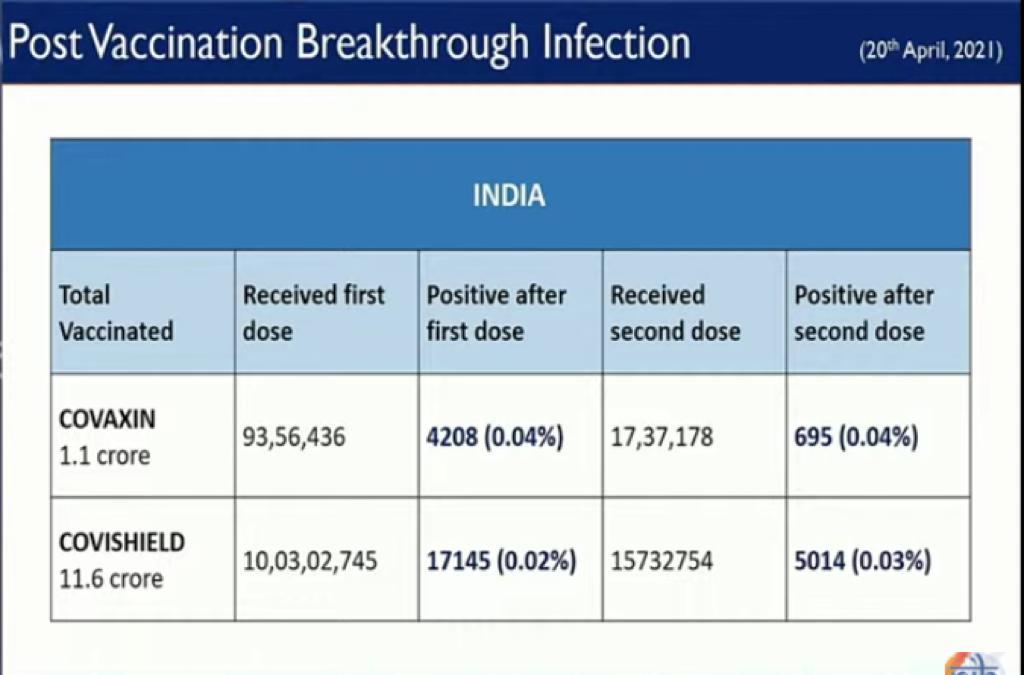
Why are some infected even after two doses?
A breakthrough infection is when someone tests positive for COVID even after being fully vaccinated. Scaremongering headlines and unrealistic expectations about the role of vaccines has exacerbated anxiety about breakthrough infections.
No vaccine is one hundred percent effective, and breakthrough infections are no surprise. Measles vaccine fails to protect about 3 percent of vaccinated individuals, and polio vaccine is approximately 80-90 percent effective. Moreover, none of the vaccines provides bulletproof ‘sterilising immunity’ that prevents people from getting infected. Vaccines are expected to block severe disease or death.

Nonetheless, unlike Covid-19, a pandemic, in the case of measles and polio, vaccinated rarely interact with infected people. Hence we see much fewer breakthrough infections in the case of polio or measles, but substantially more in Covid-19.
The good news is most breakthrough infections usually result at the best mild symptoms, and only in rare cases severe disease or death. A study conducted in Los Angeles County among vaccinated and unvaccinated as the Delta variant surged from May 1 through July 25 showed that the risk of infection among the unvaccinated was five times more than the vaccinated. The hospitalisation was around 29 times more than the vaccinated. Further, the breakthrough infection appears to be more among the elderly, whose immune system is weak due to age and among medical professionals who are constantly exposed to the virus. Thus the vaccines were seen to be effective even to the immune escape delta variant.
The delta and its sub-lineage appear to be the main driver behind breakthrough infections in India. Vaccinating a large population quickly and preventing the uncontrolled spread of the virus is the only way to slow down the evolution of the newer variants.
Take-home message: Even if you are unlucky to get a breakthrough infection, thanks to vaccination, your disease is more likely to be mild, and your chance of survival is much greater.

